
Mark E. Epstein, DVM, DABVP, CVPP
Carolinas Animal Pain Management
TotalBond Veterinary Hospital Forestbrook
3200 Union Road
Gastonia, NC 28056
Articles by Mark E. Epstein, DVM, DABVP, CVPP







Dr. Mark Epstein looks at what can result in this maladaptive pain state in veterinary patients.

A wider population of patients may be affected than previously thought.
Dr. Mark Epstein explains why these pain control mediciations remain an excellent option in many cases.

To make your pain control measures top-notch, construct a scaffold of appropriate pain medications.

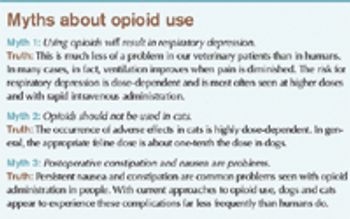
Synthetic opioids are powerful, useful tools to manage pain for one simple reason: Receptors for naturally-occurring opioids (endorphins, enkephalins) are distributed ubiquitously throughout the body and can be found in both central and peripheral tissues.

It is now a settled matter that the adaptive capacities of animals, coupled with the innate biases of human observers, seriously impairs our ability to "know" which of our patients are in pain, how much they are in pain, and sometimes, even where they are in pain.

Pain can be protective, but through the stress response it may also contribute significantly to patient morbidity and even mortality. Anxiety may contribute directly to the hyperalgesic state through cholecystikinin-mediated "nocebo" effect.

In the last 10 years, the veterinary profession has undergone what can only be described as a sea change in perspectives about animal pain and pain control. A 1993 evaluation of a veterinary teaching hospital surgical caseload revealed only 40% of patients that had undergone highly invasive, painful procedures (including orthopedic repair, thoracotomy, and intervertebral disc decompression) received any sort of pain control, and then only based on clinical signs.

The framework of effective pain management systems rests solidly on the foundation of recognition/assessment, pre-emption, and using multiple modalities. Multiple modalities allow for intervention at several different places of the nociceptive pathway, increasing effectiveness and minimizing the need for high or protracted doses of any one particular drug.
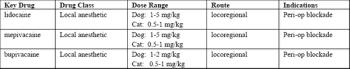
Local anesthetics were once a mainstay of pain management in veterinary medicine, and may now be one of the most under-utilized modalities. Administered locally or regionally, they are the only modality that renders complete anesthesia to a site, i.e. no transmission of nociceptive impulses as long as the drug exerts its effect.

The framework of effective pain management systems rests solidly on the foundation of recognition/assessment, pre-emption, and using multiple modalities. Multiple modalities allow for intervention at several different places of the nociceptive pathway, increasing effectiveness and minimizing the need for high or protracted doses of any one particular drug.
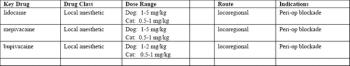
Local anesthetics were once a mainstay of pain management in veterinary medicine, and may now be one of the most under-utilized modalities. Administered locally or regionally, they are the only modality that renders complete anesthesia to a site, i.e. no transmission of nociceptive impulses as long as the drug exerts its effect.

It is now a settled matter that the adaptive capacities of animals, coupled with the innate biases of human observers, seriously impairs our ability to "know" which of our patients are in pain, how much they are in pain, and sometimes, even where they are in pain. Historically the absence of behaviors easily associated with pain (crying, whimpering, etc.) has been equated with the absence of pain.

The framework of effective pain management systems rests solidly on the foundation of recognition/assessment, pre-emption, and using multiple modalities. Multiple modalities allow for intervention at several different places of the nociceptive pathway, increasing effectiveness and minimizing the need for high or protracted doses of any one particular drug.

Synthetic opioids are powerful, useful tools to manage pain for one simple reason: Receptors for naturally-occurring opioids (endorphins, enkephalins) are distributed ubiquitously throughout the body and can be found in both central and peripheral tissues.

Dr. Mark Epstein reviews local blocks and strategies for effective administration.
Adopting a pain management culture can benefit all stakeholders involved in patient care.
Dr. Mark Epstein gives his thoughts on feline pain management.

A new strategy to extend the duration of local anesthesia may markedly help patients with moderate to severe surgical injury. Implantation of a catheter into the surgical wound site prior to closure allows repeated or continuous infusion of local anesthetics into the affected area.

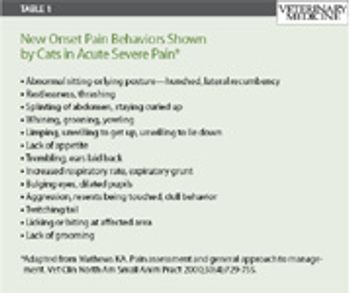
Cats add an extra dimension of difficulty when it comes to assessing pain in animals. Listed below, are just some of the "new onset pain behaviors" shown by cats in acute severe pain. (adapted from Karol Matthews's excellent chapter in the Veterinary Clinics of North America Small Animal Management of Pain, July 2000 Vol 30 issue entitled: Pain Assessment and General Approach to Management). However, the observer must be very astute if they are to pick up signs of moderate or mild pain, and are exhibited not by the onset of new behaviors, but rather absence of usual behaviors.

The good news is that veterinary clinicians are faced with a staggering array of possibilities to prevent and manage pain in surgical patients. The bad news is that veterinary clinicians are faced with a staggering array of possibilities to prevent and manage pain in surgical patients.

Rapid advances are being made in understanding the neurobiology of pain, which in turn reveal potential new targets for prevention and treatment.

Local anesthetics were once a mainstay of pain management in veterinary medicine, and may now be one of the most under-utilized modalities. Administered locally or regionally, they are the only modality that renders complete anesthesia to a site, i.e. no transmission of nociceptive impulses as long as the drug exerts its effect.

Pain can be protective, but through the stress response it may also contribute significantly to patient morbidity and even mortality. Anxiety may contribute directly to the hyperalgesic state through cholecystikinin-mediated "nocebo" effect.
Latest Updated Articles
 CVC Highlight: How I assess postsurgical pain in cats
CVC Highlight: How I assess postsurgical pain in catsPublished: December 1st 2010 | Updated:
 Pain management: The positive effects on your practice and patients
Pain management: The positive effects on your practice and patientsPublished: February 1st 2011 | Updated:
 Neuropathic pain, Part 2: Conditions that cause pain signals to go awry
Neuropathic pain, Part 2: Conditions that cause pain signals to go awryPublished: February 1st 2012 | Updated:
 Neuropathic pain in veterinary patients, Part 1
Neuropathic pain in veterinary patients, Part 1Published: January 1st 2012 | Updated:
 CVC Highlight: Opioids: The good, the bad, and the future
CVC Highlight: Opioids: The good, the bad, and the futurePublished: December 1st 2011 | Updated:
 Cutting edge interventions: Intravenous and intrawound local anesthesia for pain control (Proceedings)
Cutting edge interventions: Intravenous and intrawound local anesthesia for pain control (Proceedings)Published: August 1st 2010 | Updated: