The postpartum mare: Managing basic problems (Proceedings)
The perinatal period in the mare is associated with many medical and surgical conditions that can be life threatening. These include retained placenta; metritis, laminitis, septicemia complex; colic, and rupture of a viscus, artery or uterus. Most are emergencies and if left unattended can have dire consequences.
The perinatal period in the mare is associated with many medical and surgical conditions that can be life threatening. These include retained placenta; metritis, laminitis, septicemia complex; colic, and rupture of a viscus, artery or uterus. Most are emergencies and if left unattended can have dire consequences. The minimal diagnostics to be performed at presentation of a sick postpartum mare should include a thorough history, a basic physical examination, rectal and uterine examination, and measurement of total protein and PCV. Ultrasonographic evaluation of the abdomen, an abdominocentesis and passing a stomach tube per os may also be indicated. Veterinarians must determine if severe pain is due to a ruptured uterine artery or is associated with a gastro-intestinal problem. In some cases, the diagnosis is made on the surgery table. The outline presented below is a guideline for differentiating and treating each condition. These notes are to be a aid in the discussion of the clinical cases.
A. Retained placenta
1. Due to the serious sequelae that are possible, retained placenta should be handled as an emergency.
Tissue breakdown and bacterial growth may lead to metritis- laminitis-toxemia
Placenta should be out in 4 hrs; retained most commonly in the non-pregnant horn
Associated with conditions that cause tissue inflammation-dystocia, placentitis, abortion and cesarean section.
Common in Friesian mares!!! Afflicted mares have low serum calcium concentrations.
Treatment should be initiated by 6 hrs postpartum; some mares may not experience problems but cause of the dire consequences that may occur it is prudent to treat all mares.
2. Principles of treatment
Evacuate uterus - atraumatic expulsion of membranes
Control bacterial growth
Prevent laminitis
3. Treatment before 6 hrs
Oxytocin
Methods of delivery and doses
Small bolus IV (10-20 IU)
Add to intravenous fluids 40-60 IU/5 L
Frequency of administration-controversial Recommend 10-20 IU every 4 hr (based on unpublished data from UF)
Antibiotics + nonsteroidal anti-inflammatory drugs if placenta has not passed by 8 to 12 hrs (length of time depends on circumstances and cleanliness); Monitor mare 1 to 2 times daily until placenta has passed.
Client education Let owner know that mare may become extremely ill; owner should evaluated every 6 hrs for depression, lameness, anorexia
Re-distension of chorio-allantois
Manual removal; placenta may tear, leaving small tags that may serve as a source for bacterial adherence; Twirl placenta and lift out of uterus, don't pull downward
4. Following removal carefully examine placenta
Know normal appearance
b. Make sure it is all present - if not perform careful aseptic evaluation of uterine lumen; Mares usually retain placenta in tips of horns
5. Treatment after 12 hrs
Systemic antibiotics + oxytocin + NSAIDS (duration depends on mare's clinical condition). Minimum antibiotic therapy 5 days. Culture uterus if mare becomes ill or if mare is ill and does not improve within 72 hrs while on antibiotics; If mare is depressed, febrile, or anoretic may need to place mare on intravenous fluids. Five L of fluids may be spiked with 40-60 IU of oxytocin and 120-150 ml of calcium gluconate (23%). Deliver slowly - 1 to 2 L/hr; If in the field administer 150 ml of calcium gluconate (23%) L of saline; follow by administration of 1 ml of oxytocin
Manual re-evaluation daily
If only small tags of placenta remain, the uterus should be lavaged with large volumes of saline; if the entire placenta is retained, it is difficult to retrieve the saline as the placenta clogs tube
Follow progress of uterine involution by physical examinations, CBC, fibrinogen concentrations, rectal examination and ultrasonograpy
6. Exercise
Commonly used drugs in the post partum mare for retained placenta and metritis
B. Metritis-Laminitis -Septicemia complex
1. Etiology - gross contamination at foaling or retained placenta; Bacterial permits absorption of endotoxins, diapedesis and peritoneal contamination.
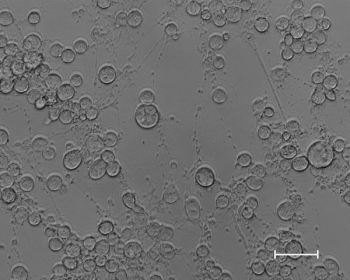
2. Clinical signs appear as early as 12 hr postpartum; fever, muddy mucous membranes, laminitis, fetid vaginal discharge, anorexia; typical clinical signs are those of endotoxemia; usually a gram negative septicemia (E Coli)
3. Management
Evacuate fluids in uterus to eliminate toxins-"saline" lavage (hot H2O with 6 oz of salt added to 12 L stainless steel bucket) or lactated ringers solution 10 L - 1-2 times a day; monitor progress of treatment by performing rectal exam before and after uterine lavage; when only a small amount of fluid has accumulated in the uterine lumen between lavages or rugae have developed decrease frequency of treatment to 1 x
b. Treat the endotoxemia-vigorous systemic therapy: antibiotics,fluids, NSAIDS, metronidazole-anaerobes are frequently recovered, polymixin.
c. Monitor medical condition by performing CBC's every 48 to 72 hrs. The total WBC count will typically drop below 3000 cells if mare has acute metritis. Numerous toxic neutrophils and immature neutrophils will be present. Fibrinogen may be > 700 mg/dl. As mare's physical condition improves, her WBC count will increase, toxic neutrophils will decrease. Decrease in fibrinogen will be by 48-72 hrs. If total WBC count is < 5000 continue uterine lavages until it rises above 5000.
d. Forced exercise unless the mare is developing laminitis then treat for laminitis (frog support; ice feet; systemic therapies vary depending on podiatrist)
C. Delayed uterine involution may lead to metritis
1. Normal rte is very fast; by 7 days postpartum the uterus is 2-3 times size of barren mare; Involution is thought to be complete by 30 days.
2. Clinical signs: uterine discharge, occasionally dull, mild pain on rectal palpation of uterus, digital pulses; Commonly occurs in mares that have to be stalled after foaling because foal is ill. Can become full-blown case of metritis.
3. Rectal findings: Large, baggy, flaccid uterus; Ultrasonography- fluid in uterine lumen; CBC-decreased neutrophil count, elevated fibrinogen, toxic neutrophils
4. Treatment
Oxytocin - uterine lavage; IV fluids spiked with oxytocin and calcium gluconate if case is severe; antibiotics; NSAIDS; Exercise
D. Necrotic vaginitis
1. Etiology-foal remains in vagina for prolonged period due to dystocia; bruising of vaginal mucosa with secondary bacterial contamination; lack of cleanliness or excessive force by operators during correction of dystocia
2. Clinical signs- may not be apparent for 3 to 5 days. Depression, reluctance to defecate or urinate; foul odor from vagina; straining tourinate; inappetence; Common in minature horses and donkeys; post dystocia
3. Diagnose by visual vaginal examination
4. Treatment - Systemic antibiotics and metronitazole; tetanus toxoid; fecal softeners; NSAID, removal of necrotic tissue may be helpful unless removal results in bleeding; if there is necrosis on the vaginal floor near the urethral opening or if the transverse folds are involved the urethral should be catheterized; be careful of uterine manipulations as may carry necrotic tissue and bacteria into uterus resulting in secondary metritis
E. Intussusception of uterine horn
1. Etiology – may occur secondary to injudicious traction on a retained placenta resulting in inversion of the tip of a horn; compromised circulation and pressure on nerve endings may produce signs of abdominal discomfort
2. Diagnose by palpation of uterus per rectum; affected horn is shortened, thickened and many times painful; If allowed to continue the horn can become necrotic or the mare may strain to the point of prolapsing her uterus.
3. Correction – fill uterus with saline or lactated ringers; rectally massage horn to replace; may place hand and arm in uterus and move arm in up and down motion similar to bouncing a basketball in an attempt to evert horn; Care must be taken not to put hand through uterine wall
4. Treatment – Systemic antibiotics; NSAID; lavage uterus;
F. Uterine prolapse
1. Etiology – secondary to dystocia, retained placenta; removal of retained placenta by pulling directly on it; may occur secondary to high doses of oxytocin (50 IU IV); can occur several hr after foaling especially if mare is straining because of another problem such as intestinal herniation, uterine rupture or eversion of the bladder
2. Treatment – Immediate – sedate or anesthetize mare, cover with sheet or plastic bag, elevate to of pelvis, cleanse with lactated ringers; gently replace with palms of hands; may be friable;
3. Primary concern- prevent rupture of large uterine vessels.
4. Treatment after replacement in abdomen – fill uterus with 10-15 L of lactated ringers or saline; siphon off; walk or jog down gentle slope; Broad spectrum antibiotics; NSAID; Intravenous fluids spiked with calcium gluconate (23%; 150 ml to 5 L lactated ringers
G. Recto-vestibular and perineal injuries at foaling
1. Etiology - result of malpositioning of the fetus, oversized fetus; overzealous assistance; heavily muscled mare (usually Quarter Horses) skittish, maiden mare that becomes frightened during foaling
2. Classification - 1st, 2nd, 3rd degree perineal laceration; rectovestibular fistulas
3. Imediate care - treat as avulsion; tetanus toxoid, keep clean, NSAIDS; antibiotics
4. Repair should be delayed until all edema and inflammation subsides at least 3 weeks; most commonly repaired after foal is weaned.
5. Prognosis- usually good; once repaired, endometritis resolves quickly
H. Cervical laceration and cervical adhesions
1. Etiology - majority due to difficult births; is also seen after abortions that occur in the 2nd or 3rd trimester; two types of tears- overstretching of muscle belly - difficult to repair; laceration of external os and part of the canal - post surgical results are fair to good for delivery of term foal; torn cervical os may adhere to the vaginal fornix thereby interfering with its ability to close properly; Mares with cervical adhesions that interfere with cervical closure will develop endometritis after breeding or may lose pregnancy in first trimester. Mares with a tear in the cervix tend to either not conceive (develop endometritis) or lose their pregnancy in the first or third trimester
2. Immediate treatment – place an antibiotic/steroid salve on the edges of the tear or roughened vaginal mucosa to prevent adhesions from forming
3. Reconstruction or removal of adhesions- evaluate health of genital tract during diestrus before deciding upon surgery; muscle belly ruptures do not generally heal well; Cervical tears or cervical adhesions located between 4 and 8 o'clock are easy to miss if exam is performed during estrus, tend to interfere with the mare's ability to carry a foal until term and most difficult to repair
I. Gastrointestinal complications associated with foaling
1. Constipation - to avoid, administer laxatives following any difficult birth
2. Bruising of abdominal viscera – compression of small colon, rectum or cecum between uterine and pelvis may result in moderate to severe signs of impaction colic and peritonitis; portion of mesentery may be torn from intestine leading to ischemic necrosis of affected segment; mare will begin to colic 6 - 48 hrs after foaling;
a) identify on rectal examination, physical examination and peritoneal tap; mare will stop defecating; mare will be painful during rectal exam; treatment includes fluids, laxatives, exercise. Outcome is dependant on severity of the esion and degree of peritonitis.
3. Rupture of a viscus - colic will occur at variable times; mare may begin to colic prior to foaling; immediately after foaling or 12 -24 hrs after foaling; most common site that ruptures is the tip of the cecum; clinical signs depend on the size and severity of the rent; septic shock may rapidly lead to death
a) Diagnosis is made by physical examination; palpation of the affected viscus per rectum-inflame serosal surface feels roughened with discernable crepitus; peritoneal tap-may recover dark green brown gastrointestinal fluid with plant material and high neutrophil count; CBC and abdominal ultrasonography
4. Large colon torsion – associated with violent colic and abdominal distention, early surgical intervention can increase survival rate
5. Rectal prolapse – associated with prolonged straining; pressure from the anal sphincter causes venous congestion and swelling which promotes more straining; may result in inschemic necrosis of the compromised bowel and peritonitis
a) Treatment – epidural anesthesia; reduce edema by gently cleansing the prolapsed section with topical glycerine or dextrose; administer fecal softeners; may need to resect bowel; impaction colic and strictures may occur after replacement or surgical repair
6. Diaphragmatic hernia-mare will exhibit severe pain that will not respond to sedatives or analgesics; mare will exhibit respiratory distress if thorax is greatly compromised; diagnose by transthoracic ultrasonography; mare may die when anesthetized
Suggested further reading
Frazer GS. Post partum complications in the mare. Part 1: Conditions affecting the uterus. Equine Vet Ed 2003;5:45-55.
Frazer GS. Post partum complications in the mare. Part 2: Fetal membrane retention and conditions of the gastrointestinal tract, bladder and vagina. Equine Vet Ed 2003; 5:118-129.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.





