
Dr. David S. Bruyette describes how to handle cats in this situation.

Dr. Dave Bruyette received his DVM from the University of Missouri in 1984 and completed an internship at Purdue University and residency in internal medicine at the University of California-Davis. He was a staff internist at the West Los Angeles Veterinary Medical Group and a member of the Department of Comparative Medicine at Stanford University. Dr. Bruyette was an Assistant Professor and Head of Internal Medicine at Kansas State University and Director of the Analytical Chemistry Laboratory at Kansas State. Currently, he is Medical Director at the West Los Angeles Animal Hospital and CEO of Veterinary Diagnostic Investigation and Consultation. Dr. Bruyette is a Diplomate of the American College of Veterinary Internal Medicine.
Two more interesting things:
1. We recommend asking Dr. Bruyette about whitewater rafting in Patagonia.
2. Dr. Bruyette is funny. Really. Very funny. So don't miss the chance to see him talk at the Fetch dvm360 conferences.

Dr. David S. Bruyette describes how to handle cats in this situation.

Two recent large studies have looked at possible environmental or dietary factors involved in the pathogenesis of hyperthyroidism.

Polyuria and polydipsia refer to excessive water consumption and urine production respectively. These are common clinical signs in both dogs and cats.

An outline of the pathophysiology, diagnosis, and treatment of hypoadrenocorticism in dogs.

Cushing's syndrome refers to all causes of hyperadrenocorticism.

Hyperadrenocorticism develops most commonly in middle-aged to older cats (mean age = 10.4 years; range 6 - 15 years).

Diabetes mellitus is a common endocrine disorder in dogs and cats. Recent data has shed light on the pathogenesis of the disorder in cats and has highlighted the role of diet and oral hypoglycemic therapy.

In the last few years it is still apparent that the best test to use in the initial approach to the patient with hyperthyroidism is measurement of total T4 concentrations.

Diabetes mellitus is a common endocrine disorder in dogs and cats.
In the last few years it is still apparent that the best test to use in the initial approach to the patient with hyperthyroidism is measurement of total T4 (TT4) concentrations.

Cushing's syndrome refers to all causes of hyperadrenocorticism with overproduction of cortisol.

Hyperthyroidism is the most common endocrine disorder in the cat.

Overview of canine hypoadrenocorticism

Polyuria and polydipsia (PU/PD) refer to excessive water consumption and urine production respectively.

Hyperadrenocorticism develops most commonly in middle-aged to older cats (mean age = 10.4 years; range 6 - 15 years).

Advances in endocrinology are happening quickly, and four areas in particular merit our attention to ensure we are keeping up-to-date and providing the best care for our patients.

Vetsulin (porcine insulin zinc suspension) is the first FDA-approved veterinary product indicated for the reduction of hypersglycemia and hyperglycemia-associated clinical signs in dogs with diabetes mellutis.

In the case of a chronic disease such as canine diabetes, we have to do an excellent job of handling clients' concerns, or it may be the owners' misperceptions about canine diabetes rather than the diabetes itsels that results in the loss of a patient. David Bruyette, DVM, DACVIM, has developed a trouble-shooting top 10 list to help assure owners of newly diagnosed dogs that it's going to be OK.

"The advantage of trilostane seems to be a much higher safety profile than Lysodren with an equal efficacy rate."

Dr. Bruyette discusses which thyroid function tests to use to diagnose hypothyroidism in dogs and hyperthyroidism in cats.

Dr. David Bruyette discusses how to optimize adrenal function testing, plus information on how to use cosyntropin.
On Dec. 31, 2005, Eli Lilly discontinued four of its insulin products: Humulin L Lente insulin, Humulin U Ultralente insulin, Regular Iletin II pork insulin, and NPH Iletin II pork insulin. Our challenges are to switch patients currently receiving these products to comparable insulin preparations and to change our treatment approach in newly diagnosed diabetes mellitus cases.

Since it was first documented in 1979, hyperthyroidism has become increasingly more common in cats.
In this article, I describe the most common clinical signs and physical examination findings in hyperthyroid cats. I also review the available diagnostic methods, including their advantages and disadvantages.

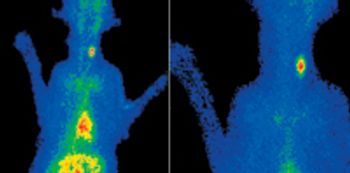
The options for treating feline hyperthyroidism include surgery, medical therapy, and radioiodine therapy.