Infectious colitis in foals and weanlings (Proceedings)
Diarrhea in young foals (< 1 month): 1) rotavirus; 2) Clostridial (difficile and perfringens); 3) Salmonella; 4) parasites (Strongyloides westeri); 5) cornavirus and 5) Cryptosporidium. Of these rotavirus, Clostridial spp. and Salmonella are the most common.
Diarrhea in young foals (< 1 month): 1) rotavirus; 2) Clostridial (difficile and perfringens); 3) Salmonella; 4) parasites (Strongyloides westeri); 5) cornavirus and 5) Cryptosporidium. Of these rotavirus, Clostridial spp. and Salmonella are the most common.
Diarrhea in older foals & weanlings:
Rotavirus, Salmonella & Clostridium spp. can still cause diarrhea in older foals and weanlings. Other differentials however should include: 1) Lawsonia intracellularis (Proliferative enteropathy) 2) other types of parasites (ascarids, small and large stronglyes).
Rotavirus
Rotavirus diarrhea is probably the most common cause of neonatal diarrhea in many species. It is species specific. It is more common in young foals, but can affect any age foal (even up to 7-8 months of life). Simultaneous infections with other viruses (coronavirus) or bacterial pathogens can also occur (and also increase severity of clinical signs).
Foals become exposed to rotavirus through other shedding/infected foals, mares, or the environment (from fecal contamination of the environment). It should be noted that the virus is very resistant to a number of disinfectants, and only phenol products (not dilute bleach!) is effective.
Clinical signs: diarrhea (mild to severe), depression, anorexia, and fever. Colic may also occur and may initially be difficult to differentiate from a strangulating lesion. Loss of electrolytes can result in hyponatremia, hypochloremia, and hyper or hypokalemia. Metabolic alkalosis can also occur. Rotavirus affects primarily the epithelial cell of the villi tip in the jejunum and ileum. A lactase deficiency results, (and a lactose intolerance), resulting in malabsorption and osmotic loss of electrolytes. Water absorption may also be inhibited because the virus inhibits a Na-D-glucose transporter.
Diagnostic Tests:
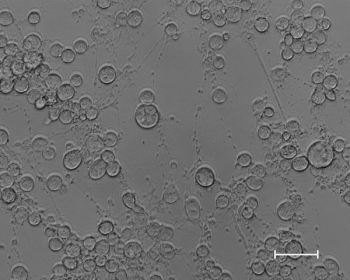
Electron microscopy will identify all the different serotypes of rotavirus, but requires 108 organisms/gm feces.
The ELIZA tests are widely used in human and veterinary medicine, and are rapid, highly sensitive and specific (Kallestad Pathfinder Direct Antigen Detection System; Premier Rotaclone Rotavirus EIA Diagnostic Kit; PorspecT Rotazyme EX Microplate Assay). The agreement between ELIZA and electron microscopy has been very good in human and equine rotavirus.
The latex agglutination (Meritec Virogen Rotatest) has been found to be more sensitive, but less specific when compared to electron microscopy.
Treatment covered at end of notes.
Prevention: There is a killed vaccine from Fort Dodge, with limited licensure (meaning that it is safe, does produce a humoral response) but efficacy is unknown. Labeled dose instructions include vaccination of the mare during gestation and 30 days prior to foaling to help produce colostral immunogloblins. Off label use could include vaccination of the mare after foaling, to help produce lactogenic immunity.
Clostridium difficile and Clostridium perfringens
Both Clostridial organisms can cause diarrhea in foals and adults. All Clostridial organisms produce exotoxins which can be very pathogenic.
Clostridium difficile produces several hydrolytic enzymes, and at least 5 toxic factors. Toxins A and B are the best described. Toxin A is an enterotoxin, and Toxin B is a cytotoxin. There are non-toxigenic strains of C. difficile, (25%) which are not pathogenic. C. difficile is highly associated with the use of antibiotics. However, it can also result in disease without antibiotic use.
Clostridium perfringensis categorized into types A-E, based on the expression of one or more lethal toxins and the combination of toxins to certain subsets. Types A and C are the most described pathogens in horses. Type C is the most severe (often fatal in young foals). Exact toxin is not as well worked out. Some labs will detect Enterotoxin unsure of the significance of this toxin.
Clinical Signs
Clinical signs of vary. The "classical" syndrome includes fatal hemorrhagic diarrhea in foals less than 7 days old. Colic, systemic sepsis, endotoxemia, and rapid deterioration are reported. However, mild diarrhea is also possible, asymptomatic carriage and shedding of the organism.
Diagnosis:
C. difficile: best done by identification of toxin (culture is difficult). Tests include 1) PCR (to test for the genes coding Toxins A and B); and 2) ELISA (for type A or types A and B).
C. perfringens: more difficult to prove. Can try to submit anaerobic culture. Some labs test for enterotoxin. Exact role of this toxin is still under investigation.
Both of these organisms and toxins can be found in normal horses and foals. Antibiotics will increase the likelihood of C. difficile. C. perfringens is isolated from almost all (90%) of 3 day old foals (and it should therefore be considered normal flora). 85% of these were C. perfringens A. In foals older than 1-2 months, and in adults, C. perfringens is found in 20-35% of horses. To note that C perfringens C was rarely isolated from normal horses and foals. In addition, Type C is associated with severe (and often fatal) diarrhea in young foals. There is no way to quickly identify Type C however.
Specific Treatment:
If foal is on antibiotics stop or consider switching. Bacitracin is not effective in horses. If specific treatment is elected (and it may not be necessary), metronidazole is the first line antibiotic of choice (10 -5 mg/kg BID to TID). However, in California, metronidazole resistant strains of C. difficile are reported, and treatment with Vancomycin has been done. Treatment with vancomycin is controversial, as it is a last resort treatment in humans.
There has been some EXTRA LABEL USE of C. perfringens type C antitoxin has been done.
Preventative measures: On affected farms, recommend foaling mares outside. EXTRA LABEL USE: some clinicians have tried vaccinating pregnant mares with Type C toxoid at 4-6 weeks, than again at 2-3 weeks prior to foaling. Injection site reactions are reported. Efficacy is unknown.
Salmonella
Salmonella is a well recognized pathogen resulting in diarrhea in all ages of horses. In foals however, Salmonella is also associated with neonatal septicemia with or without diarrhea. The clinical signs of Salmonellosis in foals can range from diarrhea, to sepsis (weakness, endotoxemia, and infectious arthritis). Salmonella (colitis and septicemia) should be suspected in foals < 30 days of age with diarrhea.
Diagnosis of Salmonella in adult horses and foals includes multiple fecal samples (5) due to the intermittent shedding pattern. There is also a PCR for Salmonella that is much more sensitive than culture. The PCR does not provide an antibiotic sensitivity or serotype. A blood culture is always indicated on any foal less than 30 days of age showing signs of sepsis and/or diarrhea (can get positive blood cultures on foals for Salmonella).
Specific Treatment: In general there is no specific treatment for Salmonellosis. Sepsis should be treated with broad spectrum antibiotics or based on sensitivity patterns.
Lawsonia intracellularis/Proliferative Enteropathy
Disease in older foals (6-12 months):
Clinical signs include weight loss, edema (due to hypoproteinemia), intermittent colic and diarrhea (but not in all cases). The clinical course of the disease can be chronic and insidious. Many of these foals will be small, and "ill thrifty". Unknown mode of transmission, likely fecal-oral and other mammals could be source.
Blood work reveals significant hypoproteinemia. There may be a leukocytosis. Ultrasound of the abdomen may reveal abnormal thick small intestinal wall (6-12 mm).
Diagnosis: Definitive diagnosis is based on biopsy/histology of the small intestinal wall. There is a cellular infiltration (usually lymphocytic/plasmacytic). Staining formalin-fixed tissues with Warthin-Starry silver stain can reveal curved bacilli in enterocytes. Further conformation requires tissue staining with IFA. Antemortem diagnosis can be based on clinical signs, hypoproteinemia, and serology from University of Minnesota. Detection of antibody is felt to be very sensitive. There is a PCR for feces; however, it is not very sensitive. In areas where the disease is more common, many practitioners may often just treat based on clinical signs (diarrhea, ill thrift, hypoproteinemia) and appropriate age (weanling).
Treatment: Many text books list macrolides such erythromycin/rifampin. The use of erythromycin is often associated with diarrhea (Clostridial especially). Use of oxytetracycline (6 mg/kg sid) and doxycycline may also be effective (10 mg/kg PO BID). In severe cases of hypoproteinemia/hypoalbuminemia the use of colloids (hetastarch) or plasma may be necessary.
General Treatment of Foal Diarrhea.
Intravenous fluids: Use of crystalloid therapy may be necessary to maintain hydration and electrolyte abnormalities. Use of intravenous fluids will require hospitalization, with many hours of nursing care. Correction of hypovolemia due to diarrhea should be corrected with either LRS, Plasma-lyte or Normosol-R (the use of saline can promote acidosis). In a very young foal (1-2 weeks of age, assume 100 lbs/50kg): bolus fluids of 1 L as frequently as 30 minutes or every 1-2 hours for the first few hours may be required to correct dehydration and improve hydration. After correction of dehydration reassessment of any acid-base and electrolyte abnormalities should be re-assessed. There is no correct formula for calculation of maintenance fluids (as some foals will continue to nurse, some will not, and volume of diarrhea lost). The maintenance fluids necessary for a 100 lb foal is approximately 3 to 5 L in 24 hours (80-120 ml/kg/day). If the frequency and volume of diarrhea is significant this will require more. Paying attention to urine output and edema formation is important! Potassium may be necessary to supplement (15-20 mEq/L). Correction of acidosis with sodium bicarbonate may also be necessary. Glucose can be supplemented to the intravenous fluids. 100 ml of a 50% dextrose solution can be added to 900 ml of LRS to make a 5% dextrose concentration. Treatment of severe hypoproteinemia may be necessary with the use of plasma or colloids (hetastarch).
Non-steroidal anti-inflammatory drugs (NSAIDs): Treatment of endotoxemia through the use of polymixin-B or hyperimmune plasma may also be beneficial during the first 48 to 72 hours.
Antibiotics? Will depend on cause, severity of clinical signs and age of foal. 1) Clostridium = metronidazole; 2) Salmonella = broad spectrum antibiotics (if positive culture- may rely on sensitivity) 3) Lawsonia = oxytetracycline, doxycycline (oral), chlorampenicol, or macrolides (clarithromycin/azithromycin) and rifampin.
Use of oral protectants: Bismuth subsalicylates (Pepto-Bismol) or Kaolin/pectin. May not be effective in moderate/severe cases. Bismuth subsalicylates may be more effective. Probably will not hurt, but may not help. "Bio-sponge® ": a commercial product that is an aluminomagnesium silicate. In vitro absorption of endotoxins and C. difficile and perfringens exotoxin has been demonstrated. There is a rationale in its use.
"Probiotic": specific probiotic – Saccromyces boulardii (25 gm/1000 horse q 12 hours)
Diet restriction: In some moderate/severe cases of clostridial diarrhea, milk restriction may be recommended. There is some rationale that toxins produce by Clostridium perfringens may exacerbate the diarrhea. If milk is restricted in a young foal, parenteral nutrition must be provided. This will require the use of a catheter dedicated just to the use of the PN or TPN (and therefore hospitalization)
Use of lactaid: Rotavirus and Clostridia diarrhea has been associated with lactose intolerance. Supplementing with Lactaid (Lactose) maybe beneficial (this can be done if the field). Lactase supplementation (6000 FCC U PO q 3-4 hours).
Determination of passive transfer & treatment of failure of passive transfer if necessary. However, many foals with Clostridial diarrhea will have good passive transfer.
Gastrointestinal ulcer prophylaxis: May or may not be necessary. In general, if the diarrhea is mild, and other treatments are minimal use of ulcer medications is unnecessary, and in some cases contraindicated in young foals. However, if the diarrhea is severe enough, the use of these drugs is probably indicated. Omeprazole (4 mg/kg for treatment, and 2 mg/kg as prophylaxis) can be done. Other anti-ulcer medications include sulcralfate and H2 antagonist (Zantac and Ranitidine).
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.





