Feline nightmare case number three: A 16-year-old cat with constipation, mild glucosuria and severe electrolyte abnormalities (Proceedings)
We were concerned about hyperthyroidism as a cause of hypertension, even with T4 in the normal range, because it is known that sick cats have falsely lowered T4's, although the free T4 should have been elevated.
Ricky is 16-year-old spayed female DSH
History
• Heart murmur detected by RDVM, referred to University of Illinois for echocardiography.
• No history of vomiting, diarrhea, PU/PD, weight loss, or inappetance.
• Ricky had been fed Hills k/d for the past year.
• On physical examination, Ricky was in good body condition, fractious, well-hydrated, with bilateral retinal detachment and a grade 4/6 systolic murmur.
• Systolic blood pressure was 260 mmHg
• Total and free T4 were both normal
• There was very mild azotemia, a serum glucose of 220 mg/dl, ALT of 133 U/L, glucosuria of 50 mg/dl, and proteinuria of 30 mg/dl.
• Echocardiogram was consistent with hypertensive cardiomyopathy, and was treated with 1.25 mg amlodipine once daily.
• Serum fructosamine was 265 umol/L (reference 175 – 400)
• The hypertension resolved within a week of amlodipine therapy, and was still controlled three weeks later, when the chemistry profile and urinalysis were repeated.
• At that time, there was no azotemia, and the urine was concentrated at 1.045, but the glucosuria had increased to 1000 mg/dl, with 30 mg/dl protein in the urine.
• Blood glucose at that time was 175 mg/dl, and the serum fructosamine was 295 umol/L.
• Over the next 2 weeks, Ricky developed constipation, and received several warm water enemas at the RDVM and at home. She was on lactulose at 1 ml PO TID. She became lethargic and anorexic at home 24 hours prior to admission to ICU.
On Presentation
• BCS 4/9
• Dull and lethargic
• Hydration appeared normal
• Large, firm feces in caudal abdomen
• 3/6 systolic murmur
• Blind
Diagnostics
• Doppler systolic blood pressure = 125 mmHg
• Urinalysis
o Spec grav = 1.045
o pH = 6
o Protein – 30 mg/dl
o Glucose – 1000 mg/dl
o No other abnormalities, no active sediment
• CBC
o Hct = 29% (reference: 30 – 45)
o Everything else normal
• Chemistry
o Phosphorus - 2.9 mg/dl ( reference: 4.0 – 7.0)
o Sodium – 134 mEg/L (reference: 144-156)
o Potassium – 3.7 mEq/L (reference: 3.9 – 5.4)
o Chloride – 100 mEq/L (reference: 112-124)
o Glucose – 167 mg/dl (reference: 65-129)
o ALT – 94 U/L (reference : 1 – 64)
o Cholesterol – 219 mg/dl (reference:63 – 130)
Problems:
• Weakness
• Anorexia
• Medically controlled hypertension of unknown cause
• Constipation
• Glucosuria
• Proteinuria
• Hyponatremia
• Hypokalemia
• Hypochloremia
• Hypophsophatemia
• Hypercholesterolemia
• Elevated ALT
Questions
What is the cause of the hypertension?
Does the cat have diabetes mellitus?
If so, why are the fructosamine results consistently normal?
What are the reasons for the electrolyte abnormalities?
What are possible causes of proteinuria in this cat?
What are possible causes of glucosuria in this cat?
Why is the cat anorexic?
Why is the cat constipated and how should it be treated?
Diagnostic/Treatment Plan and Outcome
We were concerned about hyperthyroidism as a cause of hypertension, even with T4 in the normal range, because it is known that sick cats have falsely lowered T4's, although the free T4 should have been elevated. Hyperthyroidism is an important cause of hypertension, and there was not evidence of chronic renal failure. The repeat T4 was below the detection limit of the assay, essentially eliminating hyperthyroidism as a possibility.
Hyponatremia, hypokalemia, hypochloremia, and acidosis can be caused by proximal renal tubular dysfunction. Failure of proximal renal tubular reclaiming of filtered solutes can also lead to urinary loss of amino acids, small polypeptides, and glucose. This could explain the glucosuria. The glucosuria was consistent despite unimpressive elevations in blood glucose and normal fructosamine concentrations. To test for proximal renal tubular disease we performed venous blood gases, and measured fractional excretion of potassium, chloride, sodium and phosphorus.
Sodium 0.09%
Potassium 26.5%
Chloride 0.11 percent
Calcium 0.18%
Phosphorus 56.5%
These results show appropriate tubular response to the electrolyte disturbances.
Venous blood gases were within normal limits. Ricky was treated with LRS, supplemented with KCl. She was given enemas of LRS and started on cisapride for the constipation.
Does Ricky have diabetes?
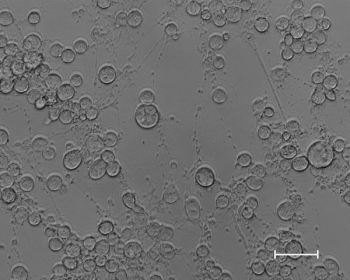
Glucose Tolerance Testing:
0.5 mg/kg glucose given IV
Samples taken for glucose measurement at 0, 5, 10, 15, 30, 45, 60, 90, and 120 minutes
We interpreted this result as glucose intolerance, and we started her on 1 U Lantus BID.
It took 10 days for Ricky's electrolyte abnormalities to stabilize, and she began eating and defecating on her own. She went home feeling fine, and continues to do well on insulin, amlodipine, and cisapride. We think the original electrolye abnormalities were due to a combination of low solute intake and over-zealous water enema administration. We're really not sure.
Her bill was $3,200.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.