Fungal diseases not just skin deep
A horse's skin and coat can be contaminated via air and soil by various fungal organisms. Though also found on normal horses, some of these fungal organisms can produce significant fungal infection under the proper conditions. From the commonly recognized ringworm to the more insidious pythiosis, horses can be infected by these potentially nasty fungal infections, which are not only irritating, but also in the case of pythiosis, can be life-threatening.
A horse's skin and coat can be contaminated via air and soil by various fungal organisms. Though also found on normal horses, some of these fungal organisms can produce significant fungal infection under the proper conditions. From the commonly recognized ringworm to the more insidious pythiosis, horses can be infected by these potentially nasty fungal infections, which are not only irritating, but also in the case of pythiosis, can be life-threatening.
Ringworm
The dermatophyte Trichophyton equinum is the most common cause of dermatophytosis or ringworm in horses, but it may also be associated with Microsporum species (M. gypseum). Ringworm is especially seen in hot, humid climates during moist, warm weather, and it is common to confined animals during fall and winter. It may be prevalent in horses in larger groups at breeding, training and racing facilities. Dermatophytes are transmitted between animals from contact with infected hair or from fungi in an environment contaminated by infected horses. Equipment such as brushes, combs, blankets and tack, all can pass an infection readily from one animal to another. Within a barn, rodents and companion animals also can spread dermatophytosis to horses.
Dermatophytosis is the only fungal disease seen with any frequency, according to Peter Ihrke, VMD, Dipl. ACVD, chief of dermatology services at the University of California-Davis. Most of their cases are Trichophyton equinum, M. canis from barn cats, and occasionally T. veruccosum from cows.
"The further south and the higher the humidity, the more dermatophytes one sees," he says.
Once exposed to the dermatophyte fungus, an infection can establish due to disruption of the skin surface of even minor abrasions, facilitating penetration and invasion into the hair follicles.
Although often seen in adult animals, young horses are especially susceptible to symptomatic ringworm infection, especially those kept indoors under poor management conditions or those horses on a poor dietary regimen.
Pythiosis lesion shows the characteristic kunkers.
Animals with immune suppression are more prone to establishment of fungal infection, such as those treated with glucocorticoids for other conditions. Horses contaminated by other skin conditions, such as prevalence of lice or those in an environment with a high incidence of biting flies. Those housed in crowded, moist or filthy conditions are highly susceptible, too. The presence of skin abrasions, however slight, or horses with areas subject to skin friction such as girth or bridle irritation, are also at risk for ringworm.
The symptoms of T. equinum usually start with patches of raised hairs in a circular or ring pattern. The hairs give way easily when plucked, and hair loss follows, leaving a silvery scaling of the underlying skin. The lesions are pruritic in the early stages of the disease but can remain sensitive to the touch for longer periods. The initial ringworm lesions can spread outward to cover large areas of the body, if no appropriate measures are taken. The disease usually resolves spontaneously within six to 12 weeks, but the fungal spores that have contaminated the stable environment and equipment can persist for years.
Signs of M. gypseum may appear suddenly as raised patches in the haircoat or as increased skin scaling in one or two spots or over the entire body surface. It then may progress to crusty, itchless and painless, patches of hair and skin one inch in diameter, spreading all over the body. It may also be localized to the lower legs, especially the pasterns. Lesions of T. equinum are usually present on the face, neck, dorsolateral thorax and girth. The legs are less commonly affected.
Because the infection is almost always follicular in horses, the most consistent clinical sign is one or many circular patches of alopecia with variable scaling and crusting, says Danny Scott, DVM, Dipl. ACVD, and William Miller Jr., VMD, Dipl. ACVD, professors at the New York State College of Veterinary Medicine at Cornell University. Some horses may develop the "classical ring lesion with central healing and fine follicular papules and crusts at the periphery."
DVM Newsbreak
Fungal culture of affected hair and scale is the most effective way to diagnose ringworm infection, to identify the dermatophyte, says Catherine Kohn, VMD, Dipl. ACVIM, professor at The Ohio State University College of Veterinary Medicine. Normal horses and those with non-fungal skin disease may be positively cultured as well as dermatophyte-infected animals.
"Where a practitioner can get into difficulty is possibly treating for something that isn't there," Kohn cautions.
Ringworm can look like sarcoids, summer sores, seborrhea, pemphigus, etc., so it needs to be identified properly.
"The antifungals are not going to be of much help if one is not treating a fungal condition," she says, so getting a skin scraping and finding the organism is a good plan prior to a treatment regimen.
Treatment
If there is an outbreak in young horses, then management must be assessed in addition to treatment. Sometimes just getting the horses out in the sunlight will speed recovery, as well as improving their plane of nutrition and deworming them. If a practitioner sees many cases within a group of young horses, isolation protocols should be instituted, and equipment should not be shared between infected and healthy horses.
"Without improving management, one is probably not going to have a beneficial outcome," Kohn says. "Considerable dollars may be spent trying to treat the disease, when improved management would help quite a bit."
If a large surface area of the horse is affected, it's harder to treat, but the main approach should be topical.
"There is a sea of antifungal agents out there, although there is little evidence as to the efficacy of any of them, so it is difficult to give advice on the choice of topical medication based on evidence," Kohn says.
The goal of the therapy is to maximize the horse's ability to respond to the dermatophyte infection, so that means correcting nutritional imbalances, concurrent diseases, and getting rid of things like systemic anti-inflammatory drugs, which might depress the horse's immune system to fight the infection.
With a few lesions, creams and lotions can be applied topically twice a day. Lime sulfur washed over the affected area is reasonably inexpensive and is easy to apply. A large spectrum of products also can be used topically, such as chlorhexidine, miconazole, niastatin cream, thiabendazole and dexamethasone.
A good thing about the rinses is that you can easily treat a larger surface area of the horse if needed, as opposed to using a more expensive cream or ointment. The animal should be bathed daily for the first week, then bathed two times a week to control the infection. The treatment with tamed iodine shampoos, chlorhexidine shampoos or 5-percent lime sulfur solutions are often effective. When bathing with shampoos, it's best to work the shampoo into the skin and allow it to soak for at least 15 minutes before rinsing, sources say.
In well-managed conditions, you're usually dealing with a few lesions on one or a few animals. The rinse can be used daily, for a week or so, and cut down on your treatment once or twice weekly until the animal is cured. That's the general approach, which may take weeks to resolve, but it's better to treat it and get it done before you put the horse in contact with other animals.
Pythiosis
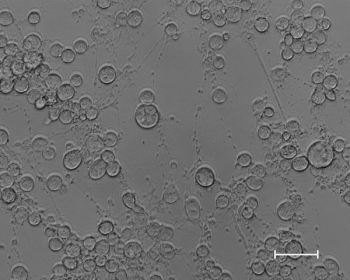
Equine cutaneous pythiosis is caused by the fungal-like organism Pythium insidiosum.
It is more common to tropical and subtropical climates, but it has also been found in Montana, Washington and New Jersey, among other states.
It is most-often associated with horses exposed to lakes, ponds and swampy areas because the organism thrives in a warmer-climate sand and requires an aquatic environment with organic substrates for optimal reproduction, says Michael Brashier, DVM, Dipl. ACVIM, associate professor at Mississippi State University College of Veterinary Medicine.
The organism grows and thrives on grass and reproduces by oospores, which travel through the water to find new grass plants. If it happens to find an animal in the process, infection can occur.
In horses, it can be an invasive, fairly rapidly progressive and proliferative pyogranulomatous disease, initially of the skin. But the organism also can invade the subcutaneous tissues. The lesions are most commonly located on the distal extremities, ventral chest and abdomen. Lesions on the lower extremities can encircle the limb and invade the tendons, ligaments and bone. The infection may be aggressive, but depending on the horse, some have lesions that grow slowly.
With some horses, small lesions can regress on their own. Once the organism invades an open skin lesion, P. insidiosum encysts, further penetrates the tissue and can enlarge rapidly. It produces an ulcerative oozing lesion with a potentially foul odor. The growing mass might be especially pruritic, and affected animals often are stressed and agitated, which might lead to self-mutilation in an attempt to relieve the discomfort. Lesions of the limbs may involve both pain and lameness due to greater tissue involvement.
"It's important to get a definitive diagnosis and not just treat empirically because there are other things that can look the same as pythiosis that should be treated differently," says Amy Grooters, DVM, Dipl. ACVIM, professor at Louisiana State University School of Veterinary Medicine.
Biopsy is important, and culture is something that is most successful using kunkers from the lesion as opposed to tissue. Culture of the causative organism is difficult, but it is critical to a definitive diagnosis. At a minimum, the lesions should be biopsied. ELISA blood tests are definitive, sources say.
"At this point in time, many equine practitioners are not aware of the disease, nor of the blood test, and therefore recognition is important," says Dawn Logas, DVM, Dipl. ACVD, of the Veterinary Dermatology Center in Maitland, Fla. "If you've got a lesion that you suspect is pythiosis, run the blood test to determine its diagnosis."
Culture is difficult because the organism does not thrive at low temperatures, and on biopsy you need a trained eye to identify the hyphal structures of the organism. If in need, Grooter's lab at LSU has special antibody stains that will pick up the hyphae and identify the organism.
"Once the lesions start, they can be locally quite aggressive and invasive and quickly invade vital structures making it impossible to completely resect," Brashier explains. "During the summer, don't just assume it is granulation tissue. Have a good look. If the granulation tissue has clefts in it with knobby pale yellow concretions in it, you need to assume pythiosis until proven otherwise because you just can't let it get ahead of you. It also tends to be quite pruritic, which simple granulation tissue isn't."
Earlier the treatment, the better
It is best to catch pythiosis and treat it as early as possible. These lesions can become as large as 30 cm in diameter. A small lesion may regress, but a larger lesion, especially on a limb, may be more difficult to treat because of the area it covers and involvement of tendon and bone, once it's established. If you have a suspicious looking lesion, do the blood test, and if it's positive, remove it, before it gets large enough to cause significant problems.
It may be treated by a combination of surgery and immunotherapy. A USDA-approved immunotherapeutic vaccine has been available since 2005.
There are various forms of surgery depending on the extent and location of the lesion, i.e. laser surgery, Grooters says. For horses, if the lesions are on the distal limbs, surgery may be difficult, where there may not be a lot of extra skin for proper closure.
"The good news about Pythium is that if you can debunk/remove the lesions, the horses do fairly well," Logas says.
To a certain degree, it depends on the location of the lesion. Those that are most worrisome are those that are on young foals, or on the limbs, which tend to invade deeper into other tissues. The result often translates into bone involvement along with cutaneous infection.
"The biggest problem we have is that Pythium is not really a true fungus or a bacteria, but an oomyces, a 'quasi-fungal' organism, and therefore classical antifungal drugs have not been effective in horses, with only mild success in dogs," Logas says. "For horses, though, the vaccine seems promising."
In horses with small lesions, pythiosis has been found to regress on its own, so whether it is the vaccine or the natural progression in certain animals is still open to question.
"It's probably going to be more effective in horses, than it is in dogs," she says. "But horses are usually able to mount a decent response anyway."
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.





