Diagnosing degrees of pain
Colic, or abdominal pain, is a relatively common problem that develops in horses of all ages. Practitioners in the field of equine medicine should be familiar with the various conditions that can contribute to abdominal pain. Once a clinical evaluation has been performed the practitioner will be able to narrow the differential list to establish a working diagnosis.
Colic, or abdominal pain, is a relatively common problem that develops in horses of all ages. Practitioners in the field of equine medicine should be familiar with the various conditions that can contribute to abdominal pain. Once a clinical evaluation has been performed the practitioner will be able to narrow the differential list to establish a working diagnosis.
With increased severity of pain, colicky horses become increasingly restless, paw the ground, lie down and roll and may groan. Severe abdominal pain is represented by sweating, violent rolling, and extreme restlessness.
Degree of pain usually correlates with the severity of clinical signs, although there is some individual variability, particularly in younger horses. This brief review will provide a basic outline of the initial clinical investigation and management of horses with abdominal pain.
Clinical presentation
Less severely affected horses may occasionally paw, look at their flank, stretch and lie down more than usual. Curling of the upper lip is considered a sign of moderate abdominal pain. Additional problems to observe include inappetance, backing to the wall, and playing with (although not drinking) water.
With increased severity of pain, horses become increasingly restless, paw the ground, lie down and roll and may groan. Severe abdominal pain is represented by sweating, violent rolling, dropping to the ground and extreme restlessness. Changes in demeanor, such as depression, should be carefully evaluated, particularly following a bout of severe colic since this may correlate with the development of endotoxemia. Alternatively, depression associated with endotoxemia occurs early in the course of disease in cases of proximal enteritis or peritonitis.
Horses suffering from strangulation obstructions generally demonstrate a progression from moderate to severe unrelenting violent pain. Severe continuous pain may be more consistent with severe tympany such as in strangulating disease where the bowel is maximally stretched or there is significant tension on the mesentery. When the degree of pain changes dramatically from severe and violent to relief or quiet demeanor, gastric or bowel rupture should be considered.
Table 1: Selected differential diagnoses for abdominal pain in horses.
Physical examination
The initial examination of a colicky horse should be considered one of the most important aspects of the evaluation, since many features of the horse's primary disease will be most apparent. For example, non-steroidal anti-inflammatory (NSAID) medications or sedative analgesic medications are commonly administered after or during examination and will alter subsequent clinical assessments.
Important components of the initial evaluation include assessments of mucous membrane color, estimated hydration status (capillary refill time, skin tent and sunken eyes), presenting heart rate, respiratory rate, borborygmi, rectal temperature and ultimately rectal palpation findings. Noting any abnormalities, or lack thereof, will provide important clues to the primary problem, and will provide the clinician with a baseline to compare to subsequent evaluations.
Historical information relevant to the presenting complaint should be thoroughly discussed with the client. Examples include signalment, housing environment, deworming and vaccination status, recent transport or stress, and nutritional status and diet (including any recent changes such as new shipment of hay or grain) and water consumption. Inquire about duration of clinical signs, severity of pain and when the horse was last observed to be clinically normal. By obtaining a thorough history, the clinician then can determine if the current problem is acute or chronic, and if any nutritional influences may have contributed to the onset of abdominal pain such as sandy paddock, poor quality hay or poor water intake.
Managing colicky horse
Following initial examination the clinician should formulate a differential list based on the primary problems that have been identified (Table 1, p. 4E). After a differential list has been considered, additional diagnostics should be performed to more definitively establish the working diagnosis. In many cases, additional diagnostics are not necessary or indicated. Examples include a relatively unremarkable examination where "spasmodic" colic is suspected or an impaction of the pelvic flexure (large colon) that is easily palpated.
In most clinical settings, a minimum database of complete blood count, serum chemistry analysis and urinalysis will provide the practitioner with valuable information relating to current metabolic status. Abnormalities identified early may relate directly to abdominal pain (e.g. elevated liver enzymes and reduced hepatic function with hepatic obstruction or inflammation) or allow the clinician to establish a baseline of where the horse was at the onset of clinical disease.
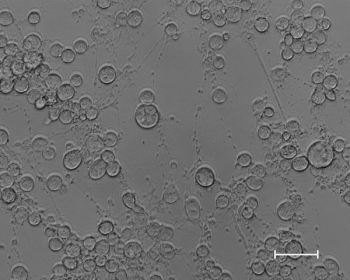
Additional diagnostic testing may include percutaneous abdominocentesis. Peritoneal fluid cytologic analysis and fluid character (color and transparency) will provide the clinician with specific information regarding the status of the abdominal environment. Good specificity and positive predictive value for color and protein concentration support use of peritoneal fluid cytology for horses with colic (Matthews, 2002). Importantly, information learned from an abnormal abdominocentesis sample (serosanguinous and/or high protein) can help stage the severity of disease, particularly when a surgical lesion is suspected.
Passage of a nasogastric tube is an important diagnostic and therapeutic strategy for evaluating the colicky horse. Whenever a nasogastric tube is passed in a horse with abdominal pain, it should be tested for the presence of gastric reflux. If reflux material is present (> 1L) then no additional fluid or laxative should be instilled into the gastric lumen. If reflux is not apparent, then water and laxative (e.g. mineral oil 5-10 ml/kg or magnesium sulfate 0.5-1.0 g/kg) are options for therapeutic purposes, a maximal volume of no more than 1-2 gallons (total) should be administered at one time.
Recent evidence supports managing relatively simple impaction-type colics with serial administration of fluids at an interval of approximately every six to 12 hours for one to several days. In some cases, management with enteral fluids is not possible (reflux or profound dehydration) and intravenous (polyionic, balanced electrolyte) fluid management is indicated. In addition, physical movement of horses is an important aspect of pain management and maintenance of adequate gastrointestinal motility, therefore frequent walking should be maintained, whenever feasible and clinically indicated.
Anti-inflammatory therapy is a major component of managing horses with colic. Flunixin meglumine (1.1 mg/kg IV) should not be administered more frequently than at 12-hour intervals. Individuals that fail to respond to this dose of NSAID may be suffering from a severe, and potentially surgical, lesion requiring further diagnostic investigation. However, mechanical obstructions such as moderate to severe colonic impactions might require multiple days of therapy until the impaction has completely resolved. Similarly, inflammatory conditions resulting in abdominal pain such as enteritis or colitis might require several days of therapy before clinical resolution is achieved. Potential complications associated with NSAID administration should be considered in colicking horses that are partially or completely fasted, stressed and potentially dehydrated. These complications include colonic and/or gastric ulceration and potentially renal (papillary necrosis) type complications.
Additional analgesic therapy for horses with colic includes the alpha2 adrenergic receptor agonists (xylazine 0.3-0.5 mg/kg IV or IM and detomidine 0.02-0.04 mg/kg IV or IM). The decision of which agent to select, typically reflects the degree of pain that is observed and temperament of the individual.
Detomidine is a more powerful and longer lasting agent that provides analgesia for up to 1 hour, in contrast to xylazine that may only provide pain relief for 15-20 minutes. The opiate agonist-antagonist butorphanol (0.05-0.1 mg/kg IV or IM) is highly efficacious for pain management in horses suffering from moderate to severe abdominal pain. Profound analgesia can be achieved when butorphanol is combined with an alpha2 adrenergic agonist (standard doses). In many cases, either agent can be administered with the initial dose of flunixin meglumine since the onset of action of flunixin meglumine requires 10-15 minutes. When sedative analgesic agents alone or in combination with flunixin meglumine are given repeatedly, this suggests a pronounced degree of abdominal pain indicating complete re-evaluation is indicated to rule out deterioration and/or a surgically correctable condition.
Horses with chronic, intermittent abdominal pain that may initially respond favorably to these basic medical therapies, yet proceed to demonstrate similar clinical signs in a period of days to weeks often require additional diagnostics. Specific examples would include abdominal radiographs for identification of a foreign body, sand accumulation or enterolith. (See Table 1.)
In contrast, young athletic racehorses may demonstrate clinical signs consistent with gastric ulceration necessitating gastroscopy for making a definitive diagnosis. Whereas abdominal abscess or peritonitis affected horses require hematology, abdominal ultrasound and abdominocentesis for a definitive diagnosis to be made. When advanced diagnostics fail to reveal the origin of abdominal pain then consider exploratory celiotomy or laparoscopy.
Colic is a dynamic process in horses, requiring frequent monitoring and potential therapeutic modification. In most cases, the presentation is straightforward and the patient responds favorably to analgesics and enteral laxative therapy. However, in a small subset of horses the condition is severe, causing unrelenting pain. In cases of moderate to severe abdominal pain, surgical intervention is commonly required; therefore, establishment of an accurate diagnosis is required for a favorable outcome. Referral is commonly required for severely affected horses, necessitating a fundamental understanding of the common presentation and progression of various forms of colic, so that the field practitioner knows the expectations for simple colic as compared to more severe, life-threatening conditions.
Dr. Davis is a 1996 graduate of the University of Florida, College of Veterinary Medicine. Following graduation she completed a rotating internship in equine medicine and surgery at Kansas State University (KSU) in Manhattan. Subsequently she completed a residency in equine internal medicine at KSU (1997-2000). She is completing her Ph.D. in equine immunology and is a clinical instructor in the KSU Department of Clinical Sciences. E-mail her at edavis@vet.ksu.edu or call (785) 532-5700.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.





