Osteoarthritis and its origins: Disease development at the cellular and molecular level
While osteoarthritis is perceived as a structural disease, the underlying pathology and chronic changes occur at a cellular and molecular level. In this article, we will discuss recent research involving the molecular mechanisms involved in osteoarthritis and newer opportunities for treatment. Key to this knowledge are research tools emerging from the scientific disciplines of functional genomics and molecular biology.
While osteoarthritis is perceived as a structural disease, the underlying pathology and chronic changes occur at a cellular and molecular level. In this article, we will discuss recent research involving the molecular mechanisms involved in osteoarthritis and newer opportunities for treatment. Key to this knowledge are research tools emerging from the scientific disciplines of functional genomics and molecular biology. Using these research tools to approach such a complex disease as osteoarthritis allows scientists to evaluate the cellular responses to the disease. Understanding the molecular events occurring within the articular chondrocyte will not only provide knowledge of the disease mechanisms, but also of new diagnostic markers and cellular targets for therapeutic and nutritional interventions.
Assessing gene-expression changes in osteoarthritis
The imbalance between anabolic and catabolic factors that leads to the breakdown and degradation of articular cartilage in osteoarthritis involves many factors at the molecular level. Many of these factors are proteins, including structural proteins of the extracellular matrix, inflammatory cytokines, catabolic and anabolic enzymes, and cell-signaling molecules. The types and amounts of proteins synthesized in the cell are specified by the expression of their respective genes. A functional genomic approach to osteoarthritis focuses on measuring changes in gene expression, allowing researchers to discover new factors involved in the disease as well as factors involved in joint tissue development or maintenance. The technologies used to measure gene expression include reverse transcription-polymerase chain reaction (RT-PCR), differential display, and microarray analysis. RT-PCR allows extremely accurate measures of specific gene transcript levels and expression differences between groups. Differential display helps visualize and isolate expression differences at a global level between two states (such as diseased vs. healthy or nutritional interventions). This gives researchers a comprehensive view of how cells respond to or are involved in a disease. Microarray technology adds the advantage of being able to quantitatively measure the expression of many genes simultaneously. However, it is limited to the genes preselected and included on the array.
Many previously known genes involved in osteoarthritis have been confirmed and novel disease genes have been identified using these technologies.1-3 Nestlé Purina has employed these research technologies to construct a microarray chip containing transcripts whose expression is altered in canine osteoarthritis and to further confirm or discover novel genes involved in canine osteoarthritis.4 One of the strengths of microarray technology is its ability to detect multiple biochemical pathways in a single sample at a single time. This ability is particularly important in a complex disease, such as osteoarthritis; the technology can potentially distinguish primary responses from disease-induced, secondary responses, as well as determine which are likely intervention candidates. Results from numerous osteoarthritis gene-expression studies suggest that inflammatory pathways play a critical role in the chondrocytes' response to injury and subsequent progression to repair or to arthritis.
RT-PCR can be used to track the changes in single gene expression, elucidating the cellular changes that arthritis induces in chondrocytes. Compared with normal cartilage, osteoarthritis-affected cartilage behaves like an activated macrophage, with up-regulation of interleukin (IL)-1, IL-6, and IL-8 gene expression. Also up-regulated in arthritic chondrocytes are prostaglandin (PG) E2, tumor necrosis factor (TNF)-α, nitric oxide, and matrix metalloproteinase (MMP)-2, -3, -9, and -13.3,5-7 These data suggest a direct connection between the elevation of these inflammatory markers and the structural changes seen in the arthritic joints, as described in the next sections.
Matrix metalloproteinases
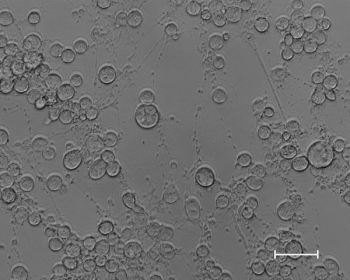
Normal articular cartilage is composed of chondrocytes imbedded in a hydrated gel of proteoglycans and a fibrous collagen framework, collectively referred to as the extracellular matrix. Chondrocytes are metabolically active cells that, among other functions, produce and maintain the extracellular matrix.8 MMPs include collagenases, stromelysins, gelatinases, and others.9,10 All these enzymes break down cartilage matrix in some manner and play an important role in the remodeling of cartilage and other connective tissues.11 In osteoarthritis, MMPs degrade glycosaminoglycans, including matrix glycoproteins, and collagen. They also reduce hyaluronic acid concentrations in the synovial fluid, leading to less viscous synovial fluid and impaired joint lubrication.10,12 Under normal conditions, the catabolic MMP processes are appropriately balanced through the inhibitory function of tissue inhibitors of metalloproteinases (TIMPs).9,11,13 However, in osteoarthritis, this balance is disrupted, with a disproportionate MMP increase.13-15
Numerous studies in dogs and other species have documented increases in active MMPs, reductions in TIMP, or both, in osteoarthritis.9,11,12,14-22 For example, researchers demonstrated that the degree of cartilage degradation in knee osteoarthritis, as determined by arthroscopy, was strongly related to the activities of MMP-2 and MMP-13 and the reduced inhibitory effect of TIMP-2 on MMP-2.11
Synovial fluid from dogs with naturally occurring osteoarthritis and dogs with rheumatoid arthritis showed higher MMP-2 activity and dramatic increases in MMP-9 activity, compared with healthy controls.15,17 MMP-9 was correlated with rapidly destructive osteoarthritis in the hip joint of women undergoing total hip replacement.19 Similarly, MMP-3 and MMP-9 were increased in blood, and MMP-1, MMP-3, MMP-9, and TIMP-1 all were increased in tissue samples from patients with this severe form of osteoarthritis.20
An increase in MMP activity is stimulated by prostaglandins, including PGE2, which may be inhibited by nonsteroidal anti-inflammatory drugs or other compounds that decrease PGE2 production.23-26
Cytokines and inflammatory mediators
Cytokines represent a major class of signaling molecules involved in osteoarthritis. They include the catabolic proinflammatory cytokines and the anabolic anti-inflammatory cytokines. These cytokines not only regulate inflammatory events, but also regulate the expression of many of the previously mentioned MMPs and other factors.
IL-1 and TNF-α are the major catabolic cytokines involved in the destruction of articular cartilage. Both are produced by synovial cells and chondrocytes. IL-1 and TNF-α increase collagen type II degradation via MMPs, decrease the expression of TIMPs, and simultaneously inhibit extracellular matrix component expression.27-29 Both of these cytokines can elicit similar responses by themselves, but together the responses are more severe. In addition to cartilage degradation, these cytokines can stimulate the expression of inducible nitric oxide synthase and cyclooxygenase (COX)-2.30,31 This results in an abnormal accumulation of pro-oxidative nitric oxide and PGE2, increasing the inflammatory response and possibly suppressing cartilage synthesis.32
In addition to PGE2, other eicosanoids are produced from arachidonic acid via the COX or 5-lipoxygenase (LOX) enzymes; these eicosanoids include thromboxane A2 (TXA2) and leukotriene B4 (LTB4) and are involved in osteoarthritis pathogenesis (Figure 1).33 The activities of these enzymes and resulting eicosanoids are increased in osteoarthritis: osteoarthritic cartilage spontaneously releases 50 times more PGE2 compared with normal cartilage.18,24,34 LTB4 promotes the synthesis and release of IL-1 and TNF-α. Further, LTB4 is a potent chemotactic agent and can increase neutrophil-induced damage to local tissues.33,35 TXA2 stimulates monocytes to release TNF-α and IL-1, which subsequently promote MMP production and joint destruction.35 PGE2 promotes local inflammation and pain. An increase in PGE2 concentration has been shown to correlate with lameness and pain in dogs with osteoarthritis.36 PGE2 can promote osteoclastic bone resorption, increased type II collagen destruction, and proteoglycans loss.23,34,37 PGE2 stimulates IL-6 release from fibroblasts, and it also sensitizes chondrocytes to free radical nitric oxide effects.33,37 COX-2 enzyme inhibition decreases PGE2 and IL-6 concentrations.37,38
Figure 1. Both nonsteroidal anti-inflammatory drugs (NSAIDs) and omega-3 fatty acids can reduce the production of eicosanoids generated via the cyclooxygenase (COX) pathway. In addition, by competitive inhibition, omega-3 fatty acids can reduce the production of proinflammatory mediators produced by 5-lipoxygenase.18,33
Altering gene-expression changes in osteoarthritis
As you can see, this inflammatory cycle is self-perpetuating, with inflammatory mediators subsequently stimulating other mediators that further the cycle. To break the cycle, one effective target has been inhibition of COX-2 enzyme-produced eicosanoids, especially PGE2. Eicosapentaenoic acid, a long-chain omega-3 fatty acid, can alter the COX-derived eicosanoids. When eicosapentaenoic acid replaces part of the arachidonic acid in cell membranes, eicosapentaenoic acid may be used instead of arachidonic acid for eicosanoid production, resulting in a different and less inflammatory set of compounds (e.g., PGE3, TXA3, and LTB5, instead of PGE2, TXA2, and LTB4). (See Figure 1.)
Eicosapentaenoic acid has been analyzed for its ability to modulate inflammatory mediators in osteoarthritis, using both in vitro and in vivo studies. Arthritic dogs fed a diet enriched with eicosapentaenoic acid had decreased MMP-2 and MMP-9 concentrations and increased TIMP-2 concentrations in synovial fluid, as well as decreased plasma PGE2.39 Likewise, in vitro studies have shown MMP expression decreases in canine arthritic cartilage in response to eicosapentaenoic acid (R.P. Middleton; S.S. Hannah: Unpublished data, 2004).
Eicosapentaenoic acid also may decrease the expression of proinflammatory cytokines and the enzymes and metabolites involved in their signaling pathways.18 This includes IL-1, TNF-α, COX-2, and PGE2. In vitro examination in our laboratory has confirmed the effect on IL-1 and PGE2 in canine cells (R.P. Middleton; S.S. Hannah: Unpublished data, 2004).
Conclusion
Osteoarthritis is a disease characterized by an imbalance in catabolic and anabolic factors affecting the degradation and synthesis of the extracellular matrix. New techniques are allowing researchers to characterize this disease and evaluate potential therapeutic agents at the cellular and molecular level. Proinflammatory mediators and inflammatory cytokines play a central role in the gene-expression changes and resulting biochemical changes seen in the arthritic articular chondrocyte. Oral eicosapentaenoic acid administration has effectively managed osteoarthritis in several species. The continued identification of the molecular mechanisms involved in osteoarthritis not only increases our understanding of the disease, but helps researchers identify and understand nutritional interventions.
References
1. Aigner, T.; McKenna, L.: Molecular pathology and pathobiology of osteoarthritic cartilage. Cell Mol. Life Sci. 59:5-18; 2002.
2. Kevorkian, L. et al.: Expression profiling of metalloproteinases and their inhibitors in cartilage. Arthritis Rheum. 50 (1):131-141; 2004.
3. Aigner, T. et al.: Anabolic and catabolic gene expression pattern analysis in normal versus osteoarthritic cartilage using complementary DNA-array technology. Arthritis Rheum. 44 (12):2777-2789; 2001.
4. Middleton, R. et al.: Gene expression profiling of osteoarthritis from canine chondrocytes. The development of a canine OA microarray chip. Trans. Orthopaedic Res. Soc.28:0741; 2003.
5. Amin, A.R. et al.: Regulation of nitric oxide and inflammatory mediators in human osteoarthritis-affected cartilage: implication for pharmacological intervention. The Pathophysiology & Clinical Applications of Nitric Oxide. (Rubanyi, G.M., ed.) Harwood Academic Publishers, Richmond, Va., 1999; pp 397-412.
6. Attur, M.G. et al.: Reversal of autocrine and paracrine effects of interleukin 1 (IL-1) in human arthritis by type II IL-1 decoy receptor. Potential for pharmacological intervention. J. Biol. Chem. 275:40307-40315; 2000.
7. Goldring, M.B.: The role of cytokines as inflammatory mediators in osteoarthritis: lessons from animal models. Connective Tissue Research. 40:1-11; 1999.
8. Johnston, S.A.: Osteoarthritis. Joint anatomy, physiology, and pathobiology. Vet. Clin. North Am. 27:699-723; 1997.
9. Cawston, T. Matrix metalloproteinases and TIMPs: properties and implications for the rheumatic diseases. Mol. Med. Today 4:130-137; 1998.
10. Roush, J.K. et al.: Understanding the pathophysiology of osteoarthritis. Vet. Med. 97:108-112; 2002.
11. Marini, S. et al.: A correlation between knee cartilage degradation observed by arthroscopy and synovial proteinases activities. Clin. Biochem. 36:295-304; 2003.
12. Tetlow, L.C. et al.: Matrix metalloproteinase and proinflammatory cytokine production by chondrocytes of human osteoarthritic cartilage: associations with degenerative changes. Arthritis Rheum. 44:585-594; 2001.
13. Hegemann, N. et al.: Biomarkers of joint tissue metabolism in canine osteoarthritic and arthritic joint disorders. Osteoarthritis Cartilage 10:714-721; 2002.
14. Kanyama, M. et al.: Matrix metalloproteinases and tissue inhibitors of metalloproteinases in synovial fluids of patients with temporomandibular joint osteoarthritis. J. Orofac. Pain 14:20-30; 2000.
15. Volk, S.W. et al.: Gelatinase activity in synovial fluid and synovium obtained from healthy and osteoarthritic joints of dogs. AJVR 64:1225-1233; 2003.
16. Clegg, P.D.; Carter, S.D.: Matrix metalloproteinase-2 and -9 are activated in joint diseases. Equine Vet. J. 31:324-330; 1999.
17. Coughlan, A.R. et al.: Matrix metalloproteinases 2 and 9 in canine rheumatoid arthritis. Vet. Rec. 143:219-223; 1998.
18. Curtis, C.L. et al.: Pathologic indicators of degradation and inflammation in human osteoarthritic cartilage are abrogated by exposure to n-3 fatty acids. Arthritis Rheum. 46:1544-1553; 2002.
19. Masuhara, K. et al.: Matrix metalloproteinases in patients with osteoarthritis of the hip. Int. Orthop. 24:92-96; 2000.
20. Masuhara, K. et al.: Significant increases in serum and plasma concentrations of matrix metalloproteinases 3 and 9 in patients with rapidly destructive osteoarthritis of the hip. Arthritis Rheum. 46:2625-2631; 2002.
21. Panula, H.E. et al.: Elevated levels of synovial fluid PLA2, stromelysin (MMP-3) and TIMP in early osteoarthrosis after tibial valgus osteotomy in young beagle dogs. Acta. Orthop. Scand. 69:152-158; 1998.
22. Tanaka, A. et al.: Expression of matrix metalloproteinase-2 and -9 in synovial fluid of the temporomandibular joint accompanied by anterior disc displacement. J. Oral. Pathol. Med. 30:59-64; 2001.
23. McCoy, J.M. et al.: The role of prostaglandin E2 receptors in the pathogenesis of rheumatoid arthritis. J. Clin. Invest. 110:651-658; 2002.
24. Martel-Pelletier, J. et al.; Cyclooxygenase-2 and prostaglandins in articular tissues. Semin. Arthritis Rheum. 33:155-167; 2003.
25. Dvorak, L.D. et al.: Effects of carprofen and dexamethasone on canine chondrocytes in a three-dimensional culture model of osteoarthritis. AJVR 63:1363-1369; 2002.
26. Pan, M.R. et al.; Non-steroidal anti-inflammatory drugs inhibit matrix metalloproteinase-2 expression via repression of transcription in lung cancer cells. FEBS Letters508:365-368; 2001.
27. Mathews, M.B.; Lozaityte, I.: Sodium chondroitin sulfate-protein complexes of cartilage. I. Molecular weight and shape. Arch. Biochem. Biophys. 74:158-174; 1958.
28. Aigner, T. et al.: Roles of chondrocytes in the pathogenesis of osteoarthritis. Current Opinion Rheumatol.4:578-584; 2002.
29. Goldring, M.B.; Berenbaum F.: Human chondrocyte culture models for studying cycolooxygenase expression and prostaglandin regulation of collagen gene expression. Osteoarthritis Cartilage 7:386-388; 1999.
30. Lotz. M.: The role of nitric oxide in articular cartilage damage. Rheum. Dis. Clin. North Am. 25:269-282; 1999.
31. Amin, A.R. et al.: Superinduction of cyclooxygenase-2 activity in human osteoarthritis-affected cartilage: Influence of nitric oxide. J. Clin. Invest. 99:1231-1237; 1997.
32. Lubberts, E. et al.: Reduction of interleukin-17-induced inhibition of chondrocyte proteoglycan synthesis in intact murine articular cartilage by interleukin-4. Arthritis Rheum 43:1300-1306; 2000.
33. Laufer, S.: Role of eicosanoids in structural degradation in osteoarthritis. Curr. Opin. Rheumatol. 15:623-627; 2003.
34. Amin, A.R. et al.: Superinduction of cyclooxygenase-2 activity in human osteoarthritis-affected cartilage. J. Clin. Invest. 99:1231-1237; 1997.
35. Cleland, L.G. et al.; Omega-6/omega-3 fatty acids and arthritis. World Rev. Nutr. Diet 92:152-168; 2003.
36. Trumble, T.N. et al.: Correlation of prosaglandin E2 concentrations in synovial fluid with ground reaction forces and clinical variables for pain or inflammation in dogs with osteoarthritis induced by transection of the cranial cruciate ligament. AJVR 65:1269-1275; 2004.
37. Bukata, S.V. et al.: PGE2 and IL-6 production by fibroblasts in response to titanium wear debris particles is mediated through a COX-2 dependent pathway. J. Orthop. Res. 22:6-12; 2003.
38. Tipton, D.A. et al.: Cyclooxygenase-2 inhibitors decrease interleukin-1 beta-stimulated prostaglandin E2 and IL-6 production by human gingival fibroblasts. J. Periodontol. 74:1754-1763; 2004.
39. Hansen, R.A. et al.: Long chain n-3 PUFA improve biochemical parameters associated with canine osteoarthritis. Proc. Am. Oil Chem. Soc., Cincinnati, May 9-12, 2004.
Newsletter
From exam room tips to practice management insights, get trusted veterinary news delivered straight to your inbox—subscribe to dvm360.