What you need to know to love diabetic cats (Proceedings)
A guide to diabetic cats.
There are five principles that greatly simplify treatment
Five principles
1) Tight control is not essential and probably not even desirable
i. Ideal for dogs: 100-200 mg/dl
ii. Ideal for cats: 100-300 mg/dl
iii. Because
a. Cats do not get significant vascular or renal disease secondary to diabetes
b. Cats do not get cataracts due to diabetes
c. Cats usually do not commit housuria
d. The toxic level of glucose is probably greater than 1000 mg/dl in cats.
2) Hyperglycemia is always better than hypoglycemia
i. The toxic level of glucose is very high
ii. But hypoglycemia kills
3) Urgency
i. As long the cat is not ketoacidotic, it is not likely to die any time soon.
ii. This principle permits us to do a one month drug trial with an oral hypoglycemic drug
iii. This principle permits us to gradually work into regulation.
4) Consistency
i. Human diabetics change their dose (and type) of insulin daily based on changing situations.
ii. We try to find the "correct" dose of insulin for cats and use it for months or years.
iii. Consistency is the basis for doing "the impossible."
5) Clinical signs are extremely important in regulating and maintaining a diabetic cat.
i. "Glycemic control is attained when clinical signs of diabetes have resolved, the cat is healthy and interactive in the home, its body weight is stable, the owner is satisfied with the progress of therapy, and, if possible, the blood glucose concentrations range between 100 and 300 mg/dl throughout the day." Feldman and Nelson' Endocrinology Text, 1996, p. 363.
Treatment of the non-ketotic, stable cat
The four steps of treatment
A. Client Education (www.greatce.com/postings)
i. Clients must participate in this disease on a long-term basis to keep the cat regulated.
ii. Clients must be educated on the following:
1) The implications to the cat
2) The implications to the owner
3) The importance of consistency
4) Hyperglycemia is always better than hypoglycemia
5) Likelihood of dysregulation
6) Spontaneous remission
7) Hypoglycemia
a. Clinical signs
b. When it occurs
c. What to do
8) Insulin
a. How and when to give
b. When to give less
9) Foods to feed and feeding schedule
10) Home monitoring
11) When to return for rechecks
B. Test for and Treat Other Diseases
i. Exocrine pancreatic insufficiency
1) Results in large volume, soft, tan stools
2) Test of choice: feline trypsin-like Immunoreactivity: fTLI
a. IDEXX; one day turnaround time
b. GI Lab, Texas A&M; 1-979-862-2861
c. 6-12 hour fasted sample required (no lipemia)
d. Also request a cobalamin (and folate) level
3) Treatment for EPI
a. Pancreazyme or Epizyme (V.E.T. Pharmaceuticals; 1-866-838-1995) with each meal
b. Do not use tablets: are not broken down rapid enough
c. Preincubation with powder does not increase the effect and decreases palatability
ii. EPI often results in cobalamin (B12) deficiency which needs to be treated.
1) Give B12 IM or SC: 250 mcg 2X per week for 6 weeks then
2) Give 250 mcg 1X per week for 6 weeks then PRN based on PLI rechecks.
iii. Chronic pancreatitis
1) There are no signs of acute pancreatitis.
2) There are no perceptible clinical signs at all.
3) The pancreatic inflammation makes it very difficult to regulate the diabetic cat.
4) About 50% of newly diagnosed cats with have chronic pancreatitis.
iv. Testing
1) fPLI is the test of choice. (pancreatic lipase immunoreactivity)
2) fPLI + fTLI increases the diagnostic yield
v. Interpretation of fPLI (October 2008; GI Lab, TAMU)
1) < 3.5: Normal
2) 3.5-5.3: Increased
3) > 5.3: Disease present
4) In general, the degree of elevation of the fPLI does not predict severity. There really is no specific degree of elevation where you could say that the cat should have clinical signs. Having said that, I believe strongly that with a serum fPLI of >/= 5.4 you would have significant disease." J. Steiner 10/08
5) This test is now available through IDEXX Laboratories with a one-day turnaround time.
vi. Treatment
1) Pancreatic replacement enzymes (Pancreazyme, Viokase) to induce negative feedback. This approach is not longer recommended.
2) Denosyl (SAMe) or Denamarin - Nutramax Laboratories – via veterinary distributors
3) Steroids: They are beneficial in diabetics with pancreatitis at low doses: 2.5-5.0 mg q24h.
4) Treatment Protocol
a. Use both drugs for 4-8 weeks then recheck fPLI.
• If it is not reduced significantly, continue both drugs for another 4-8 weeks then recheck the fPLI.
• If it is less than 5.3 mmol/L, discontinue Denosyl and continue prednisone for another month.
• Some cats never achieve normal values. If their diabetes is well controlled, either discontinue prednisone and Denosyl or continue just prednisone.
5) If the f PLI and fTLI are elevated, treat the underlying inflammation. An elevated fPLI and fTLI is not justification to euthanize the cat.
vii. Treat existing infections
1) Bacterial infections are common in diabetics (pyelonephritis, cystitis, cholangiohepatitis, periodontitis, etc.)
2) If they are not controlled, regulation is nearly impossible.
3) Treat with a broad-spectrum antibiotic for 1-2 weeks: Clavamox alone or Clavamox + Zeniquin if serious.
4) Determine if the teeth need to be cleaned
a. If so, treat for 1-3 weeks with insulin, stop to clean teeth then resume regulation process
C. Diet
i. High fiber diet
1) Slows transit time of food through the gut leveling the peaks and valleys of bG values.
2) Traditional high fiber diets are high in carbohydrates.
3) This approach is obsolete.
ii. Low carbohydrate diet
1) Also high in protein, fats, and calories
2) Differences in cats and dogs
a. Cats are not equipped to handle high carbohydrate loads.
b. They are obligate carnivores, unlike dogs and humans.
c. Thus, dog and human dietary rules do not apply to the diabetic cat.
d. In dogs, hexokinase and glucokinase are responsible for glucose phosphorylation in the liver, trapping glucose in the liver to be metabolized.
e. Cats have no hepatic glucokinase activity so glucose cannot be metabolized easily.
f. Amino acids are the cat's building blocks for gluconeogenesis. They are powerful secretagogues.
g. Thus, cats continuously produce glucose to maintain proper blood glucose levels.
h. There are no blood glucose "peaks and valleys" like dogs.
i. When deprived of food for several days, cats break down muscle as an amino acid source for producing glucose.
j. They maintain normal blood glucose levels even during starvation.
3) Purina's DM Formula
a. A low carbohydrate, high protein, high fat, high calorie diet.
b. Canned and dry.
• There are higher remission rates when the canned food is fed exclusively.
c. Extremely palatable
d. Indications (The D Diet)
• Diabetes, Delicious, Debilitated, Development, Diarrhea, Dermatophytosis
e. Contraindications
• Renal failure: high protein = high phosphorus levels
• Obesity in a non-diabetic cat
• When alkaline urine is needed (It acidifies the urine.)
o Renal disease (tendency to acidosis; high protein = high phosphorus)
o History of calcium oxalate urolithiasis
o Hypercalcemia
iii. Reduced carbohydrate, high fiber
1) Purina's OM – reformulated in 2005 (reduced carbs, higher protein, high fiber)
2) My choice for the multiple cat household where all cats must eat the same thing and one is diabetic.
iv. However, consistency is more important even than the right diet.
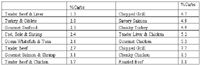
Comparisons of "low carbohydrate" diets and others
Dry matter basis

Fancy feast canned products
Percent carbohydrates – Dry matter basis
Revised 8/08
Low carb diets
D. Insulin
i. There are many valid reasons to begin insulin first:
1) Minimize glucose toxicity
2) Preserve β-cell function
3) Greater chance of remission
4) Better control
ii. Choices for the non-ketoacidotic cat
1) Amino acid sequences
a. The closer the amino acid sequence, the less likely for an immune reaction (antibody formation)
b. Beef is one amino acid different from Feline
c. Pork is one amino acid different from Canine.
d. Human is several amino acids different from Feline and Canine.
2) PZI: beef/pork (Boehringer Ingelheim)
a. 90% Beef + 10% Pork
b. Long-acting
c. U-40 concentration
d. Wholesale cost ~ $79/bottle
e. U-40 syringes required (~$20 per box of 100)
f. When FDA approved, a new recombinant PZI product, will be sold by Boehringer-Ingelheim.
3) Humulin N
a. Intermediate acting
b. Human-cell origin
4) Vetsulin
a. 100% Pork
b. Approved for dogs
c. U-40 concentration
d. Used in cats with reasonable success.
5) Glargine (Lantus®): See Editorial in J Vet Int Med. April 2006
a. Very good response in diabetic cats
b. Give q12h; much better than q24h (although q24h is an option when essential)
c. Better on virgin diabetics than PZI based on rates of remission
d. U100 concentration; use 0.3 U100 syringes; consider a syringe magnifier
e. Do not dilute; any change in pH inactivates the drug.
f. ~$75 per bottle retail
g. DNA recumbent; therefore, no antibody production
h. "Discard after 28 days" per package insert.
• An opened bottle is good for 30 days when stored at room temperature.
• An opened bottle is good for 6 months when stored at refrigerator temperature
• Discard if there is any discoloration: due to bacterial contamination or pH change.
• Use of the entire bottle could result in 200 withdrawals from the bottle increasing the risk for contamination.
i. Observations by Dr. Jacquie Rand (www.uq.edu.au/vetschool/centrecah)
• "Many cats have negligible glucose lowering effect in the first 3 days (do not increase dose), although by day 10 after beginning insulin, most cats have good glycemic control."
• "For many cats, the time at which the nadir (lowest) glucose concentration occurs is often not consistent from day to day, or between cats. Sometimes it occurs between the two doses, but sometimes the nadir occurs around the time of the next dose."
• "Most commonly the highest glucose concentrations occur in the morning and the lowest in the evening."
• "Some cats consistently have their nadir glucose concentration in the evening just before the next insulin injection, and less commonly, it occurs around the time of their morning injection."
• "It is a very common observation by owners that when long-term stable diabetic cats are changed over to glargine, usually they do better clinically, even if blood glucose results do not support the clinical improvement."
iii. Gradual Regulation
1) If initial bG < 400 mg/dl (22 mmol/l): Begin with DM food or glipizide or both (borderline diabetic)
2) If initial bG > 400 mg/dl (22 mmol/l): 2 U BID SC for most 8-10# cats
3) I do not try to regulate in the hospital
a. It is difficult to get them to eat well.
b. It is difficult to get them to change their diet.
c. Their activity level will change greatly when they go home.
d. A new dose of insulin takes 5+ days to give consistent results.
e. Because their appetite and activity change when they go home, they are no longer regulated.
f. It is a great waste of client dollars that could be better spent on the proper insulin and diet.
4) Treat for ~7 days then recheck at 12 hours post-insulin (without insulin being given).
a. Goals
• Resolve clinical signs
• Blood glucose = 300-350 mg/dl (16.5-19.5 mmol/l)
5) Record
a. Hours post insulin
b. Weight [compare to previous]
c. Clinical signs
d. Blood glucose
6) If the bG is < 350 mg/dl (19.5 mmol/l), continue this dose for another 1 week then recheck. It is probably regulated.
7) If the bG is > 350 mg/dl (19.5 mmol/l), increase to 3 U BID and repeat in ~7 days.
8) When the bG is < 350 mg/dl (19.5 mmol/l), continue this dose for another 1 week then recheck. It is probably regulated.
9) Each time you recheck the cat, check more than just the bG.
a. If the bG and the clinical signs conflict, believe the clinical signs.
b. You may also use a fructosamine on these cats, but the cat should be on a consistent dose of insulin for 1 week to get a reliable result.
10) Glucose testing
a. Abbott's AlphaTRAK is calibrated for cat and dog blood; RECOMMENDED
b. It is not calibrated lower than actual, as is the case with all human glucometers made for home use.
c. But even the best glucometers will not give consistent results on the same blood sample.
The glucose curve
a. The glucose curve is unsuccessful if:
i. The dose is changed from the last 5 days
ii. The cat does not eat
iii. The cat experiences hyperglycemia due to stress: This happens in a significant number of cats.
b. Summary
i. Do a glucose curve if feasible and use the results if they are really a curve and if they do not conflict with the clinical picture.
ii. HOWEVER, I NO LONGER DO GLUCOSE CURVES.
1) JAVMA, 2/1/03
2) JAVMA. 4/1/07
c. Why they don't work in cats
i. The effects of stress hyperglycemia
ii. Most commercial cat foods contain complex CHOs that are broken down slowly.
iii. Cats nibble so CHO intake is dispersed throughout the day.
d. Fructosamine
i. Represents the average glucose reading for 1 week
ii. The stress of today's hospital visit is averaged so it does not affect the result significantly
iii. The time of day of blood collection is not important
iv. Anesthesia may be used for blood collection
v. Shortcoming: Somogyi Overswing (rebound hyperglycemia)
vi. Interpretation:
1) 110-300: Not diabetic (for diagnosis of diabetes)
2) 190-350: Excellent Control
3) 350-450: Good Control
4) 450-600: Fair Control
5) Over 600: No Control
6) (Antech Lab: If 200-400: Good Control)
e. New data on fructosamine in cats (Link & Rand, JFMS, 12/08)
i. Fructosamine equals a mean bG for about one week.
ii. Cats with persistent moderate hyperglycemia (~310 mg/dl; 17 mmol/l) did not consistently have elevated fructosamine levels. Fructosamine cannot reliably be used to diagnose these cats (DM vs. stress hyperglycemia). Dehydration and hyperproteinemia lower fructosamine levels. A dehydrated or hyperproteinemic diabetic cat may have a normal fructosamine level. When using the fructosamine level for confirming/diagnosing diabetes, be sure to consider the clinical signs of PU,PD,PP, WL. Cats that are diabetic have these clinical signs, even if the owner has not observed them.
iii. There is a wide range of plasma fructosamine values associated with a given blood glucose concentration. It is not as precise and repeatable as we would like it to be. In the study, cats with a bG = 523 ± 5 mg/dl (29 mmol/l) had fructosamines of 400-633 µmol/l. Those with a bG = 310 ± 7 mg/dl (17 mmol/l) had fructosamines of 292-378 µmol/l.
iv. The critical difference for fructosamine values is 33 µmol/l. When doing sequential fructosamine values, a change less than 33 µmol/l is not due to a change in bG levels.
v. Changes in fructosamine values as great as 120 µmol/l may occur with no change in bG concentration.
vi. Ketoacidosis may produce higher fructosamine values than expected based on bG concentrations.
vii. "Therefore, serial plasma fructosamine concentrations in an individual cat over time may provide more useful information on diabetic control, rather than attempting to extrapolate a mean glucose concentration from the plasma fructosamine concentration."
Oral hypoglycemics
a. Only for non-insulin dependent diabetics
b. Cats progress from non-insulin dependence to insulin dependence over time
c. Therefore, the success of glipizide is short-term
d. I only consider using it for borderline diabetics when DM alone is not successful.
E. Dose
i. Begin at 2.5 mg/10# BID for one week
ii. Recheck bG and clinical signs (clinical signs improve much more than bG)
iii. If no response, increase to 5 mg/10# BID for 3 weeks
iv. Check bG weekly
v. May increase to 7.5 mg/10# TID and give for weeks ?? months ??
f. Side-effects
i. Vomiting/anorexia
ii. Hypoglycemia (very unlikely)
iii. Hepatotoxicity
iv. Side-effects generally avoided by starting at the 5 mg BID dose for the first week.
Dysregulation
a. Four Important Issues
i. Is the cat really dysregulated or does it just have bad bG readings?
ii. Owner issues: insulin handling, insulin administration, time of day, consistency issues
iii. Other disease present: infections, hyperthyroidism, Cushing's', acromegaly
1) Acromegaly testing
a. Insulin-like Growth Factor-1
• Michigan State University (see below)
• 1 cc serum (or plasma); performed on 2nd and 4th Wednesdays; $40.00 your cost
• Sensitivity = 84%; Specificity = 92%
• Normal range: 12-92 mmol/L; > 200 mmol/L strongly suggestive of acromegaly
b. Serum Growth Hormone level
• Increases sensitivity and specificity if both tests performed
• Performed at U MN, Veterinary Diagnostic Laboratory, (800) 605-8787; vdl@umn.edu
• Currently only performed once per month due to low demand; should change.
• www.vdl.umn.edu/ourservices/guidelinefiles/endocrinology/home.html#growth
• $40 your cost.
c. I recommend both tests when: dysregulation, owner is compliant, AND insulin dose is 9+ U BID.
i) Insulin incompatibility due to antibody formation.
2) Insulin antibody level
a. Diagnostic Center for Population and Animal Health, Michigan State University, (517) 353-0621, download submission form from: www.animalhealth.msu.edu.
b. Diagnostics
i. Verify dysregulation
ii. Check consistency issues
iii. Blood profile, PLI, insulin antibody
iv. Urinalysis and urine culture
v. Check teeth
vi. Give antibiotics for 1 to 2 weeks
Miscellaneous tidbits
Periodontal disease
a. Insulin dose can decrease up to 25% after teeth cleaning and antibiotics.
b. Clean the teeth as soon as possible, even before regulation is achieved.
Surgery on a diabetic cat
A. For short procedures
i. Follow the rule: hyperglycemia is always better than hypoglycemia
ii. Feed the cat at 4-6 pm the day before surgery and give one-half dose of insulin
iii. Give no food or insulin the morning of surgery
iv. Use an anesthetic that permits rapid recovery (isoflurane or sevoflurane by mask then via endotracheal tube)
v. Give one-half dose of insulin at the first feeding, then the full dose at the next feeding
Managing the hypoglycemic crisis (Norsworthy protocol)
a. Three Steps
i. Rapidly increase the blood glucose
ii. Give 1 tablespoon of corn (Karo) syrup now; repeat in 20 minutes; if no response: IV treatment
iii. IV dextrose (25 or 50%) slowly IV to effect (approx. 1 ml of 50% per kg)
iv. Continue dextrose therapy for 24+ hours
v. IV 5% dextrose preferred or food (high protein)
vi. Determine why it happened before resuming insulin
vii. If cause cannot be determined, assume spontaneous remission
viii. Stop insulin for 24 hours then check blood glucose to see if the cat is still diabetic.
Transient diabetes and spontaneous remission (JVIM, JAN 99)
a. Transient DM occurs because subclinical diabetes is present. These cats often have pancreatic pathology that results
i. in decreased islet cell density (~50% of normal). A state of insulin resistance occurs due to steroids, Ovaban,
ii. hyperthyroidism, etc. Treatment normalizes the cat allowing spontaneous remission to occur. It occurs slowly but
iii. it presents as a severe hypoglycemic crisis. Client education is the key to early recognition. The occurrence is 15-
iv. 20% of diabetic cats. Diabetes almost always recurs.
Scales for weighing cats: Pelouze model 4010 (150 pounds); 1-800-498-0017; www.businesssupply.com
When your client is out of town for the weekend, determine what to do with the cat based on the consistency principle.
The most common cause of death in diabetic cats is: _________________________________ .
Norsworthy's eight steps to diabetic success
1. Educate your clients.
2. Don't in a hurry with non-ketoacidotic cats.
3. Treat other diseases.
a. Especially pancreatitis and periodontal disease.
4. Use PZI.
5. Feed DM.
6. Don't try to regulate non-ketoacidotic cats in the hospital.
7. Don't do glucose curves.
8. Look at the cat.