Staging and management of canine chronic kidney disease
Chronic kidney disease (CKD) occurs over a period of months to years and is a leading cause of morbidity and mortality in dogs.
Chronic kidney disease (CKD) occurs over a period of months to years and is a leading cause of morbidity and mortality in dogs. Nephron damage associated with CKD is usually irreversible and can be progressive. Whether the underlying disease primarily affects glomeruli, tubules, interstitial tissue, or renal vasculature, irreversible damage to any portion of the nephron renders the entire nephron nonfunctional. The histologic appearance of CKD caused by different primary diseases is often similar since the healing of irreversibly damaged nephrons occurs by replacement fibrosis. It is usually not possible to improve renal function in CKD; therefore, treatment is aimed at stabilizing renal function. Increasing evidence indicates that dietary and antihypertensive/antiproteinuric treatments can decrease the progressive nature of canine CKD.
The pathophysiology of CKD can be considered at both the organ and systemic level. At the level of the kidney, the primary pathology of CKD is loss of nephrons and decreased glomerular filtration. Reduced glomerular filtration results in increased plasma concentrations of substances that are normally eliminated from the body by renal excretion. In addition to excretion of metabolic wastes and maintenance of fluid and electrolyte balance, the kidneys also function as endocrine organs and catabolize several peptide hormones. Therefore, hormonal disturbances also play a role in the pathogenesis of CKD. For example, decreased production of erythropoietin contributes to the nonregenerative anemia of CKD and decreased metabolism and excretion of parathyroid hormone and gastrin contribute to osteodystrophy and gastritis, respectively. Finally, part of the pathophysiology of CKD is brought about by compensatory mechanisms like the hyperparathyroidism that develops in an attempt to maintain normal plasma calcium and phosphorus concentrations. Similarly, the individual glomerular filtration rate of intact nephrons increases in CKD in an attempt to maintain adequate renal function; however, proteinuria and glomerulosclerosis may be consequences or trade-offs of this hyperfiltration.
Due to the interdependence of the vascular and tubular components of the nephron, the end point of irreversible glomerular or tubular damage is the same. Morphologic heterogeneity between nephrons exists in the chronically-diseased kidney with changes ranging from severe atrophy and fibrosis to marked hypertrophy. Progressive diseases that destroy nephrons at a slow rate allow intact nephrons to undergo compensatory hypertrophy, which can delay the onset of renal failure (persistent azotemia superimposed on the inability to concentrate urine). Therefore, when renal failure finally occurs, nephron hypertrophy can no longer maintain adequate renal function and usually < 20 percent of the original nephrons are functional. Renal diseases that have been associated with the development of CKD in dogs include glomerulonephritis, amyloidosis, tubulointerstitial disease, pyelonephritis, nephrolithiasis, leptospirosis and neoplasia.
Staging CKD
Many different terms have been used to describe renal disease and decreased renal function. Unfortunately, these terms can be confusing due to lack of standard definition and application. For example, there are no uniform definitions for terms like "early renal disease," "renal insufficiency," or "end-stage renal disease." Recently, a staging system for CKD was proposed by the International Renal Interest Society (IRIS). This group consists of approximately 20 independent veterinary nephrologists from ten countries with the mission of helping practitioners better diagnose, understand, and treat canine and feline renal disease. The following system was developed by the IRIS Board in order to improve communications surrounding CKD and link appropriate diagnostic and therapeutic efforts to patients with varying stages of CKD. This staging system has been adopted (after input and modification) by both the American and European Societies of Veterinary Nephrology and Urology (see Table 1).

Table 1 Stages of Chronic Kidney Disease (CKD)
This system uses serum creatinine concentrations as the major determinate for the four stages. Serum creatinine concentrations should always be interpreted in light of the patient's urine specific gravity, body condition score, and examination findings in order to rule out pre- and post-renal causes of azotemia. In addition, the staging system should only be applied to dogs with stable CKD since in other forms of renal disease (e.g., acute renal failure or acute decompensation of CKD) the plasma creatinine concentration can change significantly over a short period of time.
The classic diagnosis of chronic renal failure based on persistent azotemia superimposed on the inability to concentrate urine pertains to CKD in later Stage II through IV. CKD that is categorized as Stage I or early Stage II CKD (nonazotemic CKD) could be diagnosed in dogs with renal proteinuria (persistent proteinuria with an inactive urine sediment), urine concentrating deficits, increases in serum creatinine over time that remain in the normal range (e.g., serum creatinine that increases from 0.6 to 1.2 mg/dL could indicate a 50 percent reduction in nephron numbers), or abnormal renal palpation or imaging findings. The above stages are further classified by the presence or absence of renal proteinuria and systolic hypertension (See Table 2).

Table 2 Hypertension and proteinuric classifications in CKD patients
Management of CKD
Treatment of CKD is ideally linked to the stage of disease (see Table 3). In Stage I and early Stage II CKD, specific treatment directed at the primary cause of the kidney disease is the primary objective (see Figure 1). While it may not be possible to identify the primary cause of the CKD, specific treatments have the potential to reduce the magnitude of subsequent renal damage. As an example, bacterial pyelonephritis can cause or complicate CKD, and this condition can be specifically treated with appropriate antibiotic therapy.

Table 3 Examples of treatments linked to stage of CKD
In many dogs with Stage II CKD, renal lesions progress and renal function deteriorates. Progression of disease, as well as the rate of decline is monitored by physical examination and longitudinal assessment of blood pressure, proteinuria, and serum chemistry values. Dietary management is an example of a so-called renoprotective treatment that has been shown to reduce the progression of CKD in dogs. In a study of client-owned dogs with Stage II or III naturally-occurring CKD, feeding a renal diet resulted in a 70 percent reduction in the relative risk of developing a uremic crisis (acute decompensation). In comparison, dogs fed a renal diet remained free of uremic signs almost two and one-half times longer and had a median survival that was three times longer than dogs fed a maintenance diet.
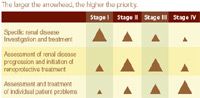
Figure 1 Prioritization of diagnostic and treatment efforts based on the stage of CKD
Reduction of dietary phosphorus is one of the cornerstones of CKD management and can be accomplished by feeding specifically formulated diets for CKD. From a practical nutrition standpoint, dietary phosphorus reduction is combined with dietary protein reduction. If after three to four weeks of dietary phosphorus restriction serum phosphorus concentrations remain high, enteric phosphate-binding agents containing calcium, aluminum, sevelamer, or lanthanum should be administered with meals (initial dosage of 30 mg/kg body weight to achieve normophosphatemia). Physiologic dose replacement of vitamin D3 (calcitriol) is the third line of defense in the treatment of hyperphosphatemia and hyperparathyroidism and has been used successfully in dogs with CKD.
Treatment of patient symptoms becomes a higher priority in the later stages of CKD when the decreased renal function has a more pronounced effect on the patient's quality of life. In addition to phosphorus restriction and protein reduction, dietary management includes omega-3 fatty acid supplementation, salt reduction, and alkalinization—all of which are designed to reduce patient symptoms and slow disease progression. Acceptance of a renal diet is enhanced with early initiation (while the patient still has a good appetite) and gradual implementation. Vomiting and anorexia are common patient symptoms in dogs with later stage CKD and can often result in decreased caloric intake. Causes of vomiting and anorexia include: 1) stimulation of chemoreceptor trigger zone by uremic toxins, 2) decreased excretion of gastrin and increased gastric acid secretion, and 3) gastrointestinal irritation secondary to uremia. Vomiting may be treated with metoclopramide, which blocks the chemoreceptor trigger zone. Metoclopramide also increases gastric motility and emptying without causing gastric acid secretion, and is one of the drugs of choice for vomiting associated with renal failure. H2-receptor blockers (e.g., famotidine or ranitidine) have been shown to effectively decrease gastric acid secretion, which may attenuate vomiting in dogs with CKD. Oral ulcers, stomatitis, and glossitis may occur as a result of gastritis and vomiting or the effect of uremic toxins on mucosal membranes and will often also result in anorexia. If vomiting has been controlled but anorexia persists, placement of a feeding tube (esophagostomy or gastrostomy tube) will often facilitate the maintenance of caloric intake and hydration status. In many stage III and IV dogs without feeding tubes, fluid therapy with polyionic solutions, given intravenously or subcutaneously in the hospital or subcutaneously by owners at home (10-50 ml/kg every one to three days), will help improve the patient's quality of life.
Dr. Grauer is professor and Jarvis chair of small animal internal medicine at Kansas State University in Manhattan, Kan. Dr. Grauer's expertise involves small animal urinary system diseases and disorders.
Podcast CE: Canine cardiology: the practical guide to the mitral valve patient
July 19th 2023Learn about the prevalence of myxomatous mitral valve disease, guidelines for staging heart disease, proactive diagnostic workup, the importance of spironolactone and aldosterone blocking, and the benefits of combination therapy for improved outcomes in canine patients
Listen