No hoof, no horse: Ending the scourge of laminitis
With a little less than three years to go, will equine researchers meet the ambitious goal of Vision 2020to conquer laminitis?

A horse with a classic laminitis stance. All images courtesy of Dr. Andrew van Eps.Laminitis-the painful, crippling disease from damage to the hoof's sensitive laminae-has been a scourge for ages, but it may soon … finally … be overcome. It is estimated that 15 percent of horses in the U.S. are afflicted by laminitis in their lifetime. Up to 75 percent of those affected eventually develop severe or chronic lameness and debilitation. An estimated $13 million annually is associated with the evaluation and treatment of laminitis and the loss of horses after a diagnosis.
In 1989, we lost Secretariat. In 2002, we lost Sunday Silence. In 2008, we lost Barbaro. The efforts to save Barbaro brought laminitis into the spotlight, raised public awareness about this dreaded disease's impact on individual horses and the equine industry, and emphasized the need to step up research and increase research funding.
An ancient disease
Laminitis, with its crippling lameness and potential for death, is not a new disease. It was reported as early as 300 B.C. Aristotle termed laminitis “barley disease,” because horses were observed to develop the disease after ingesting excessive amounts of barley. Another ancient laminitis report was published upon the order of Roman Emperor Constantine in A.D. 900. It listed several possible causes, including the horse traveling on hard surfaces, overeating and drinking too much cold water when hot.
Now in 2017, there is reason for hope. Veterinarians at major universities worldwide are working on and inching closer to a cure. We're on the verge of being able to treat the early stages of laminitis and perhaps reverse its devastating course that leads to the demise of so many horses.
“I've studied laminitis for nearly 20 years, and I'm finally becoming optimistic,” says Andrew van Eps, BVSc, PhD, associate professor of equine musculoskeletal research at the University of Pennsylvania School of Veterinary Medicine's New Bolton Center.
The Vision 2020 effort of the veterinary community is working to make “meaningful progress toward conquering laminitis by 2020,” according to Rustin Moore, DVM, PhD, DACVS, chair of the Department of Veterinary Clinical Sciences at The Ohio State University College of Veterinary Medicine.1
So how are researchers doing?
Getting closer
“When I look back at when Barbaro was at New Bolton Center [2007-2008], I'm amazed at how little we knew about laminitis,” Dr. van Eps states. “We know so much more now. During those years, real evidence-based scientific research on the mechanisms of different forms of laminitis was just gaining momentum. Around the time of Barbaro's hospitalization, we were starting to measure blood insulin, but we really had no idea about it. We were just starting to come to grips with the fact that different types of laminitis existed.”
Dr. van Eps explains that there are three different etiologies:
- Endocrinopathic laminitis, which is associated with endocrine dysfunction and increased blood insulin
- Supporting-limb laminitis, which develops in the contralateral limb of horses with a painful limb condition
- Sepsis-associated laminitis, which occurs secondary to systemic inflammatory disease.
According to Dr. van Eps, equine veterinarians are better equipped to intervene because they're more aware of the mechanisms involved in each type of laminitis. “I think we're close to solving the laminitis problem,” he says. “Research groups around the world have been making progress uncovering the pathways that lead to laminitis.”
The New Bolton Center team-which consists of Dr. van Eps; senior research investigator Hannah Galantino-Homer, VMD, PhD; and associate pathology professor Julie Engiles, VMD-is actively researching laminitis pathophysiology. “We have the benefit of some strong collaborations with researchers like Belknap at OSU,” Dr. van Eps says. James Belknap, DVM, PhD, DACVS, has been researching laminitis mechanisms at the tissue level at The Ohio State University. “These collaborations really accelerate the rate of discovery.”
Endocrinopathic laminitis
Dr. van Eps says researchers are close to identifying why laminitis occurs secondary to endocrine disorders that lead to increased blood insulin-conditions such as Cushing's disease, pituitary pars intermedia dysfunction and equine metabolic syndrome. “Some horses and ponies inherently produce a lot of insulin in response to ingested carbohydrates, particularly from grazing pasture,” he says. “We're close to identifying why high blood insulin causes the changes in the lamellar tissue of the foot itself, which creates the disease. … We're looking at different ways to directly block those processes from happening.”
A major part of that approach is to address the underlying endocrine issue. “If we can address those problems, we can manage laminitis and prevent it from worsening,” Dr. van Eps says. “In previous years we never thought that was possible.” Now he thinks it's possible even to reverse early laminitic changes in some horses and ponies if the issue is caught early and the underlying endocrine disease is carefully controlled.
Supporting-limb laminitis
Dr. van Eps is also optimistic about being able to effectively intervene and prevent supporting-limb laminitis in clinical cases. This is the kind of laminitis that affected Barbaro. “Preventive strategies are more achievable than we had previously thought,” Dr. van Eps says. “In the last couple years, we have made some significant inroads into identifying why supporting-limb laminitis happens and how we can prevent it. We're garnering convincing evidence that supporting-limb laminitis is a blood perfusion problem associated with load. Specifically, the loss of normal limb load cycling patterns appears to be the problem.”
Researchers are learning that when horses preferentially place weight on a limb, it directly interferes with blood flow to the hoof (see Figures 1 and 2). To properly perfuse the lamellar tissue in the hoof, the horse must cycle weight on and off the limb, Dr. van Eps explains. When a horse puts a lot of weight on a leg, it appears that they need to cycle that leg even more frequently than normal. Clinicians can help with that.
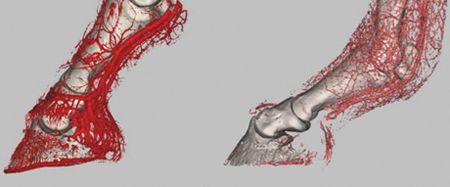
Figure 1. CT scan contrast arteriography of an unloaded (left) and loaded (right) limb. This demonstrates the effects of weightbearing on vascular patency in the equine distal limb, relevant to supporting-limb laminitis.
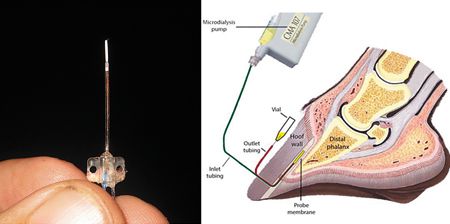
Figure 2. Tissue microdialysis. For this technique, a tiny probe (left) is inserted into the tissue, allowing measurement of substances including energy metabolites in the interstitial space. It has been adapted to the lamellar tissue of the equine hoof (right), allowing researchers to examine blood flow and energy balance in different situations, including weightbearing load. Research is showing that increased weight load combined with a reduced frequency of weight shifting appear to cause negative energy balance, leading to supporting-limb laminitis. Researchers are using the technique to help identify practical methods to prevent this.“We're starting to recognize effective interventions to prevent supporting-limb laminitis and are currently testing these,” Dr. van Eps says. “These involve providing partial, intermittent relief of weight-bearing on the support limb. The key is knowing where the threshold is, how frequently and how much relief we have to provide.”
Dr. van Eps says preventing supporting-limb laminitis can help orthopedic surgeons truly save many injured horses. “Surgeons like [Dean Richardson, DVM, DACVS, of Penn's New Bolton Center] can fix jigsaw-puzzle fractures like Barbaro's,” he says. “But despite this amazing work, these horses still succumb to supporting-limb laminitis. I was a resident when Barbaro was at New Bolton Center. A lot of what I do today and much of the research my colleagues have done on supporting-limb laminitis are a result of Barbaro and his owners Roy and Gretchen Jackson. Fittingly, this work supports his legacy.”
Dr. van Eps says believes that his team's current work will lead to the ability to prevent weight-bearing laminitis. “I'm encouraged that there are achievable results on the horizon,” he says.
Sepsis-associated laminitis
The laminitis type that has been studied most is the kind that develops in horses that are systemically sick with endotoxemia or sepsis. “And yet,” Dr. van Eps says, “we probably know the least about exactly why this happens.” In people with sepsis, organ failure is common. And although septic people don't develop laminitis, they do develop lung injury or kidney failure. Human medical researchers don't know why organ failure occurs in sepsis.
Equine practitioners do know that this type of laminitis can often be prevented by cooling the feet. There is good clinical evidence for this approach, particularly in cases of diarrhea and colitis. “We recently published studies that looked closer at the mechanism that explains why cryotherapy works,” Dr. van Eps says. “It probably has to do with slowing the metabolic rate within the lamellar tissue itself. We used to think cryotherapy simply inhibited inflammation, but our recent research shows that's not necessarily the case. The intent has always been to identify exactly why cryotherapy works, and then come up with a practical pharmaceutical intervention.”
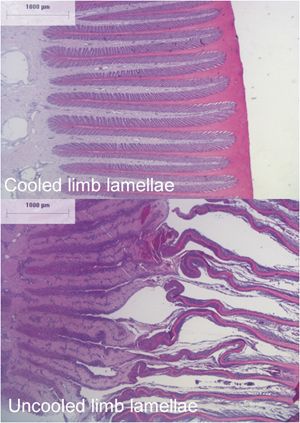
Figure 3. Histology shows remarkable preservation of the lamellae in the cooled limb (top) compared with the uncooled limb (bottom). Research is uncovering the mechanisms by which cooling exerts its protective effects. The aim is to discover more clinically practical means of laminitis prevention and early treatment.Although it seems that cryotherapy should be a fairly easy procedure to perform, Dr. van Eps notes that it's actually quite difficult to administer continuously over long periods. Horses treated properly with cryotherapy are typically in a teaching hospital environment.
Dr. van Eps witnessed the transition from those days when cooling the feet was not routine and newer treatments had not been developed for horses with diarrhea, pneumonia or retained fetal membranes. “About 25 percent of those horses would founder, which could be career-ending or life-threatening,” he says. “Now it's much less common for these horses to develop severe laminitis if they receive appropriate treatment. We have improved our treatment of the primary disease, but I think cooling the feet has also helped stop laminitis in those cases.”
Dr. van Eps notes that he has seen dramatic reductions in inflammatory cytokine production occur when researchers cooled horses' feet experimentally. But when his team applied foot cooling as horses began to show the onset of clinical laminitis, “it didn't affect the inflammatory cytokines at all,” he says. Still, there was a dramatic effect in preventing progression. “Since it didn't affect inflammatory occurrence, the question is, what is it affecting?” he says. “We still don't 100 percent know.”
Dr. van Eps says that in human sepsis, researchers think systemic disease may affect the energy metabolism of tissues in various organs, resulting in dysfunction. “In a recently published study, we have evidence that cold therapy slows metabolism in the lamellar tissue of horses in a sepsis-type model, reduces the demand for nutrients and more tightly regulates the energy metabolism of the tissue in a way that protects it from sepsis-induced metabolic dysfunction,”2 Dr. van Eps says.
The promise of laminitis research
Dr. van Eps is encouraged that clinicians are close to being able to diagnose the different forms of laminitis earlier than they could previously and to treat, prevent and even reverse the disease. Researchers are zeroing in on the cellular mechanisms involved-processes that disrupt the normal attachment of lamellar tissue to hoof and bone.
What's more, awareness of the different types of laminitis has changed the way veterinarians think about clinical cases. “With most endocrine-associated laminitis in horses and ponies, early intervention and tight control of the underlying endocrine issue is the absolute key,” Dr. van Eps says. “With sick horses, we can prevent laminitis by cooling their feet, even though we still don't know exactly why this works.”
During the past 10 to 15 years since Barbaro's death, much has been discovered about laminitis, and practitioners are taking steps to successfully manage it in clinical settings. “This is the first time I've been so optimistic about finally enabling the equine veterinary profession, as Vision 20/20 states, to ‘conquer the different forms of laminitis by 2020,'” Dr. van Eps says. “It's really exciting!”
Acknowledgment
Dr. van Eps and his team would like to thank the Grayson-Jockey Club Research Foundation, which has funded laminitis research at the University of Pennsylvania New Bolton Center since 2009. For more information on supporting this work, visit grayson-jockeyclub.org.
Reference
1. Moore R. Vision 20/20: Conquer laminitis by 2020. J Eq Vet Sci 2010;30(2):74.
2. van Eps AW, Poulsen L, Belknap JK. The effect of continuous digital hypothermia on lamellar energy metabolism and perfusion during the development of laminitis in the oligofructose model. Eq Vet Ed 2017;29(S8):38.
Suggested reading
1. Belknap JK, Geor RJ, eds. Equine Laminitis. Oxford, UK: Wiley-Blackwell, 2017.
2. van Eps A, Collins SN, Pollitt CC. Supporting limb laminitis. Vet Clin North Am Eq Pract 2010;26(2):287.
3. van Eps A, Orsini JA. A comparison of seven methods for continuous therapeutic cooling of the equine digit. Eq Vet J 2016;48 (1):120.
4. van Eps A. Therapeutic hypothermia (cryotherapy) to prevent and treat acute laminitis. Vet Clin North Am Eq Pract 2010;26(1):125.
5. van Eps A. Progress towards effective prevention and therapy for laminitis. Eq Vet J 2012;44(6):746.
Ed Kane, PhD, is a researcher and consultant in animal nutrition. He is an author and editor on nutrition, physiology and veterinary medicine with a background in horses, pets and livestock.