How veterinarians can address atrial fibrillation in horses
As long as they don't have more serious heart disease such as CHF, most horses under a veterinarians care do well with intervention through pharmacologic or electrical cardioversion.
Atrial fibrillation (AF), an electrical disorder of the heart rhythm, is the most common pathological arrhythmia in horses. With this condition, the atria fail to contract but instead quiver or fibrillate, and impulses are conducted intermittently through the atrioventricular (A-V) node to the ventricles. The resulting electrocardiogram (ECG) has irregular R-to-R intervals, a lack of P waves and undulations in the baseline—known as F waves—that are caused by the fibrillating atria (see Figure 1).
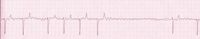
Figure 1. An ECG tracing showing atrial fibrillation, characterized by a lack of P waves, irregular R-to-R intervals and undulating baseline F waves. (Photo courtesy of Laura Faulker, VMD, New Bolton Center.)
Although AF often develops in horses with advanced structural heart disease—particularly in horses with valvular insufficiency that results in atrial dilatation—horses often develop this arrhythmia with minimal or no detectable signs of heart disease.
"We see a broad spectrum of horses with AF, including a young racehorse that has no other cardiac disease that we can detect but has acute onset of AF," says Virginia Reef, DVM, DACVIM, University of Pennsylvania's New Bolton Center. "Such horses are considered similar to what they call lone AF in humans, which is AF in an otherwise healthy heart." Reef also sees horses that have AF associated with underlying structural disease. Mitral regurgitation is the most common valvular insufficiency causing left atrial enlargement, and these horses are at more risk of developing AF, she says.
"In older horses with AF that aren't engaged in vigorous work, we suspect that they might have underlying myocardial disease even if we can't definitively identify it," Reef says.

If a horse with atrial fibrilation (AF) has a highly athletic job, such as polo, the horse needs to be treated for AF to perform safely, experts say. (GETTY IMAGES/THOMAS HOTTNER)
A small group of horses also present with AF and congestive heart failure (CHF). "That category of horse we would treat very differently," says Reef. For horses with CHF, AF is not the primary problem. Instead, it's the underlying heart disease that is causing the CHF, and treatment focuses on rate control and palliative treatments rather than rhythm conversion.
Which horses are affected—and how
AF typically affects full-grown horses. "Fortunately, AF is rare in foals, though occasionally you'll have a newborn foal have a transient arrhythmia," Reef says. "You need a critical atrial mass to get AF, so it isn't a problem in foals, basically, unless the foal has a very diseased heart." For the same reasons, AF is not a problem typically seen in ponies, unless their hearts are enlarged.
Just as horses with AF vary between those with healthy hearts and those with CHF, the presenting complaint in horses with AF can vary widely as well. High-level athletes, such as race horses, event horses, polo ponies, fox hunters, barrel racers, endurance horses and many show jumpers, experience exercise intolerance and a drop in performance. Horses that perform at lower level cardiovascular work, such as dressage horses, show hunters, Western pleasure horses and trail or pleasure horses, may not have any signs of AF that their owners can detect. The reason for these different presenting signs involves the physiology of horses with AF.
During the cardiac cycle, the atria depolarize and contract, and then, subsequently, the ventricles depolarize and contract. The atria prime the pump, or the ventricles, which are responsible for moving blood to the lungs and to the body.
"If the atria are fibrillating, you've essentially lost that prime to the pump," says Reef. "At rest that does not make any difference whatsoever, though during exercise it makes a big difference, as priming of the pump might contribute 15 to 20 percent of cardiac output."
If the horse is doing intense athletic work, optimum cardiac output is important. Cardiac output is determined by both heart rate and the amount of blood moving out of the ventricles at each heartbeat (stroke volume). AF decreases stroke volume during exercise, resulting in a higher heart rate at each level of exercise.
Young, healthy horses in normal sinus rhythm can have heart rates of 240 beats/min or even higher during maximal exercise. Horses with AF, however, have a heart rate typically 40 to 60 beats/min higher at each level of exercise, so they often reach that maximal heart rate at a submaximal exercise level.
"With that irregularity of rhythm, and the lack of that priming of the pump, it seems that horses in AF cannot do their job if their heart rate exceeds 220 beats/min, for whatever the exercise level that they're doing," says Reef.
At New Bolton Center, if an owner is considering not treating a horse for AF because it is not exhibiting clinical signs, then an exercising ECG is obtained to ensure the horse is safe to perform its job while it is experiencing AF. Some horses do not follow the general rule of being just 40 to 60 beats/min higher than average, and these animals can have dangerously high heart rates just trotting. Others exhibit malignant ventricular arrhythmias in addition to AF during exercise. Cardioversion is recommended for these horses if their owners wish to continue to use them as performance animals.
Treatment options
Three treatment options are available for AF in horses, with the exception of horses with CHF:
1. Pharmacologically converting the arrhythmia, with the most common drugs being either quinidine gluconate or quinidine sulfate
2. Performing a transvenous electrical cardioversion (TVEC) procedure, which was originally designed at the University of Guelph, Ontario, and also developed at the University of Ghent, Belgium
3. Not treating the arrhythmia and leaving the horse in AF.
As for the first two options, Reef says that there are no data or controlled studies that conclude that one is better than the other. "Though there are some known risks with the use of quinidine, there are also risks with TVEC," she says. And the third option? "Many horses doing low level exertion can perform their jobs just fine in AF," Reef says.
How do you determine which treatment to recommend to the owner? If a horse has a highly athletic job such as racing, three-day eventing, polo, rigorous fox hunting or upper level show jumping, that horse needs to perform safely at a relatively high level of cardiovascular work. "One needs to choose either the pharmacologic or the electrical cardioversion, because those horses could not do their job without it," Reef says.
In addition, there is a subset of horses that, although their performance is not that demanding, cannot do their job safely while in AF because they have excessively high heart rates or ventricular arrhythmias. "When the heart rate gets very high, they are also more at risk for developing ventricular arrhythmia," says Reef. That situation could possibly lead to sudden death, though it is rare. Still, you don't want people riding these horses, Reef says.
"If you have a horse that is a low-level competition horse, you need do an exercise test to determine if it is safe to use as intended," Reef says. The owner may decide not to treat the horse if it's safe for his or her purposes. But if the horse has a high heart rate or ventricular arrhythmias, if it's involved in rigorous exercise and needs to compete at the top of its game, if it's a sales prospect, or if the owners want to do what's best for the horse long-term, an owner may decide to convert the arrhythmia even if the horse isn't experiencing any clinical signs, Reef says.
Pharmacologic cardioversion
Reef says that if a horse is carefully monitored, quinidine is reasonably safe when used by experienced clinicians. And the pharmacologic use of quinidine administration is probably half the cost of TVEC.
"Any antiarrhythmic drug that one would administer to convert AF—quinidine being the most common—has the potential of making the arrhythmia worse," says Reef. There are other side effects, most commonly relating to the gastrointestinal tract, that one has to look out for.
For AF, the administration of quinidine sulfate has been approved for more than 30 years. The average dose is 22 mg/kg (10 g/450-kg horse) given every two hours until a normal sinus rhythm is achieved, the horse experiences an adverse reaction or a total of four doses has been administered. Most horses will tolerate four of those doses every two hours and convert sometime in the following two hours. So if you calculate that four-dose regimen, the average horse will convert within eight to 10 hours.
Several other medications have been tried to treat AF in horses, but those other drugs have more side effects and are less efficacious than quinidine.
"There are a fair number of private practices that will use quinidine, but what we do at New Bolton Center is more closely monitored," says Laura Faulkner, VMD, of the New Bolton Center. "We have a continuous ECG on the horses all the time during treatment, as well as once they are discharged home. We also take periodic plasma quinidine concentrations to see if the quinidine concentration is within the therapeutic range or is getting too high and close to a toxic level, and then we adjust our treatments accordingly. That is why we feel quite comfortable doing quinidine cardioversion because we can monitor the horses so closely."
Reef adds, "New Bolton Center is one of the few places that can actually evaluate plasma quinidine concentrations in a real-time situation and use the information to treat the horse most effectively. The quinidine blood-to-tissue equilibration occurs very quickly—within 30 minutes. If the horse has not converted with the initial treatment every two hours and is tolerating the treatment well, we continue with quinidine administration every half-life (i.e., every six hours), to maintain a steady-state plasma and tissue concentration of the drug. This regimen is often successful in horses with chronic AF. By maintaining a steady-state plasma concentration of the drug, you are giving the heart time to convert."
In private practice, or in facilities that can't monitor plasma quinidine concentrations, clinicians use a pulsatile treatment with quinidine—give several doses, then stop and not treat the horse overnight, then resume the pulsatile treatment in the morning. With this method, the horse is more likely to get toxic concentrations of the drug in its tissues and blood and it may experience more side effects.
Electrical cardioversion
There is a subset of horses that need electrical cardioversion because quinidine places the horses at more risk. "Within that patient population, quinidine allows the heart to conduct more of the fibrillating impulses to the ventricles," Reef says. "And then the horses' heart rates can get way too high and they can be at risk for other arrhythmias."
Horses normally have very high resting vagal or parasympathetic tone that slows impulse conduction through the A-V node. But this influence is lessened in very excitable or nervous horses, and, thus, their resting heart rate in AF may be elevated. These horses may also have sympathetic-induced ventricular arrhythmias. Quinidine enhances conduction through the A-V node, which can result in dangerously high heart rates in certain horses. Therefore, excitable, nervous horses, or those with ventricular arrhythmias, are ideal candidates for electrical cardioversion.
"TVEC is used in horses because administration of external defibrillator paddles, as per human medicine, is not successfully used in horses," says Reef. With TVEC, two electrodes are passed via two separate catheters through the jugular vein into the horse's heart. One is directed to the left branch of the pulmonary artery, so it is sitting over the left atrium, while the other inserted into the right atrium.
"The idea with TVEC is to have the electrical current go across the fibrillating atria to reestablish that normal rhythm," Reef says. The catheters must be placed properly; placement is done under echocardiographic guidance, and thoracic radiographs are obtained to ensure the catheters are properly placed.
The amount of time it takes to place a catheter, administer anesthesia, perform the TVEC procedure and recover the horse varies from facility to facility, says Reef: "It's a shorter time frame than a quinidine cardioversion, but it takes many more people to do it." The procedure requires both expertise and specialized equipment, such as the proper defibrillator, so TVEC procedures are performed only at specialized facilities such as teaching hospitals and advanced equine facilities. This need for specialized equipment and several personnel makes TVEC more expensive than pharmacologic cardioversion.
"Some of the risks with TVEC are just the fact that horses have to be under general anesthesia. And with horses, more than with other species, there are risks of general anesthesia, especially during recovery," says Faulkner.
"The key is to weigh both the client's concern for the TVEC procedure—which includes the risk of general anesthesia, recovery, all those issues—versus the drug administration," says Reef.
Prognosis after AF conversion
The prognosis is generally good for affected horses without more severe heart disease. "An important point is that if you successfully cardiovert a horse in AF back to normal sinus rhythm by any method, the horse should be able to go back to a healthy state," says Reef. "That is one of the great things about treating horses with AF—you can restore the horse to its previous performance activity. It is a very successful treatment. The horse's ability to convert—to go back to 'normalcy'—and go back to race successfully or to whatever athletic performance event it is required to perform is independent of the way you decided to treat it. Once the horse's heart rhythm is normal, the horse is good to go."
Ed Kane, PhD, is a researcher and consultant in animal nutrition. He is an author and editor on nutrition, physiology and veterinary medicine with a background in horses, pets and livestock. Kane is based in Seattle.
Suggested reading
> Faulkner L. 2012. A horse with heart. Available at: http://www.vet.upenn.edu/PennVet/News/PennVetExtraArchive/Pilotstory/tabid/2447/Default.aspx.
> Young L, van Loon G. Editorial: Atrial fibrillation in horses: new treatment choices for the new millennium? J Vet Intern Med 2005;19:631-632.
> The equine heart: power plant unequaled! CEH Horse Report, March 2012. Available at: http://www.vetmed.ucdavis.edu/ceh/docs/horsereport/pubs-March2013-sec.pdf.
> Fenton FH, Cherry EM, Kornreich BG. Termination of equine atrial fibrillation by quinidine: an optical mapping study. J Vet Cardiol 2008;10:87-103.
> Verheyen T, Decloedt A, van der Vekens N, et al. Ventricular response during lungeing exercise in horses with lone atrial fibrillation. Equine Vet J 2013;45:309-314.
> Reef VB, Levitan CW, Spencer PA. Factors affecting prognosis and conversion in equine atrial fibrillation. J Vet Intern Med 1988;2:1-6.
> Reef VB, Reimer JM, Spencer PA. Treatment of atrial fibrillation in horses: new perspectives. J Vet Intern Med 1995;9:57-67.
> McGurrin MK, Physick-Sheard PW, Kenney DG. Transvenous electrical cardioversion of equine atrial fibrillation: patient factors and clinical results in 72 treatment episodes. J Vet Intern Med 2008;22:609-615.
> De Clercq D, van Loon G, Schauvliege S, et al. Transvenous electrical cardioversion of atrial fibrillation in six horses using custom made cardioversion catheters. Vet J 2008;177:198-204.