How to approach pet dental care year-round
Veterinary teams can incorporate oral health into their practice 1 evidence-based bite at a time
Do you feel that placing all your dental eggs into February, National Pet Dental Health Month, leaves the other 11 months of the year jealous? If so, consider embarking on a yearlong dental journey, dedicating each month to plunge into a specific dental subject. This, akin to eating a large meal 1 bite at a time, allows for a deeper understanding of each discipline’s complexities, evidence-based therapeutic strategies, and evolving paradigms.
An introduction to various areas of dental care with suggestions for each month are as follows:
Month 1: Periodontal diseases
Why is this important?
Periodontal disease, incited by plaque, is the upregulation of inflammation leading to the progressive destruction of tooth support affecting 80% of dogs.1 Embracing diagnostics and therapeutic approaches tailored to each stage of periodontal disease will be time well spent, effectively managing and preventing this common ailment.
What to know
- There are 4 recognized stages of periodontal disease, each with specific diagnostic criteria and treatment.
- Using a diagnostic test alerting to the presence of thiols (caused by gram-negative oral bacteria) incorporated into every wellness visit will result in greater awareness (Figure 1).
Figure 1.

- Periodontal disease is preventable.
- The stages of periodontal disease are as follows:
- Stage 1: Gingivitis
- Mild inflammation and redness of the gingiva; slight bleeding on probing.
- Treatment: professional dental cleaning to remove plaque and calculus (tartar), followed by diligent home care with brushing (or wipes) and daily Veterinary Oral Health Council (VOHC)—approved dental product use.
- Stage 2: Early periodontitis
- Diagnosis/treatment: supragingival and subgingival scaling, polishing, and irrigation, followed by probing to assess pocket depths or attachment loss. Home care remains crucial to decrease the progression of the disease.
- Stage 3: Moderate periodontitis
- With tooth support loss, diagnosis can be made with probing and intraoral radiographs showing bone loss between the cementoenamel junction and the apex.
- Treatment: advanced gingival surgery or extraction of the affected teeth.
- Stage 4: Advanced periodontitis
- Many patients experience tooth support loss diagnosed through probing and intraoral radiographs and through-and-through furcation exposure.
- Treatment: extraction
- Stage 1: Gingivitis
Early intervention and consistent daily (or better, twice daily) home care with VOHC-accepted dental wipes, water additives chews, and tooth brushing as well as twice-yearly dental checkups and care can significantly reduce periodontal disease progression and its associated health risks.
Month 2: Tooth resorption
Why is this important?
Most pet owners will have their animals examined semiannually to help them have longer and healthier lives.2 Tooth resorption affects approximately 30% of mature dogs3 and over 50% of adult cats.4 Resorption becomes painful once the lesion progresses to oral cavity exposure.
What to know
- Tooth resorption is progressive and classified with 5 anatomic stages3 and 3 radiograph types. The radiograph types dictate treatment.
- Therapy options include follow-up, extraction, or coronectomy with gingival closure, depending on the clinical and intraoral radiograph findings.
- Tooth resorption is considered to be progressive.
Root replacement resorption is diagnosed radiographically (Figure 2A), with decreased root opacity compared to adjacent teeth and lack of periodontal ligament space. This type 2 root resorption can be successfully treated with coronectomy and gingival closure, isolating the root from the oral cavity, which allows continued replacement with bone. Extraction is the treatment for all other forms of root resorption (types 1 and 3) that have either compromised the tooth or are exposed to the oral cavity (Figure 2B).
Figure 2A: Intraoral radiograph appearance of stage 2/ type 1 root resorption.
Figure 2B: Extracted canine tooth affected with stage 3 tooth resorption.
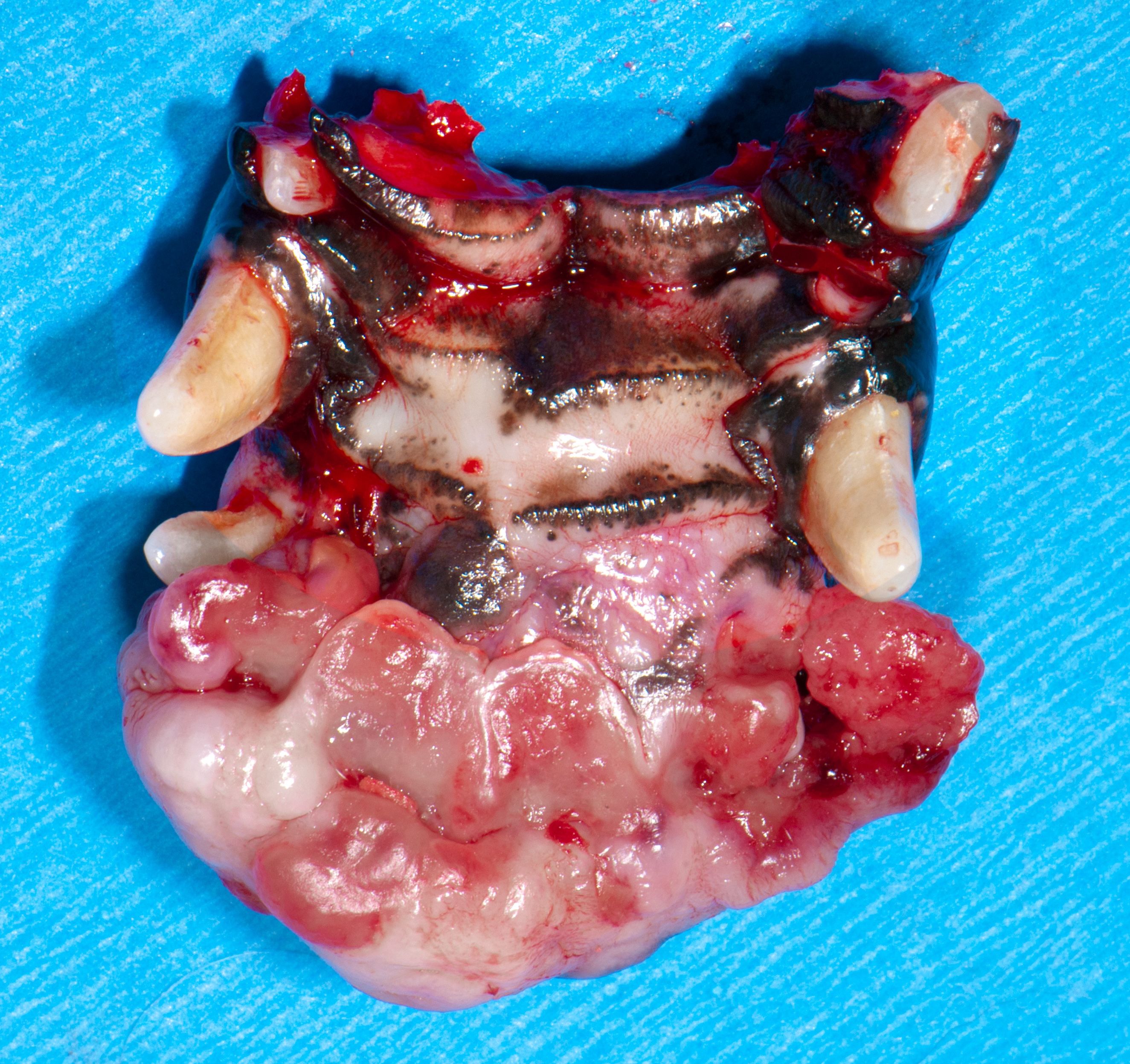
Month 3: Stomatitis
Why is this important?
Marked generalized gingival and oral mucosal inflammation is termed stomatitis. Its etiology is multifactorial, implicating plaque. Extraction of the cheek teeth or all teeth and subgingival root fragments is curative in many cases in approximately 60% of cases (Figure 3). Carbon dioxide laser ablation and alternate-day prednisolone are often helpful in refractory cases.5
Figure 3.
The extraction of teeth caudal to the canines resulted in a cure.
What to know
- When caudal oral cavity inflammation is present, the prognosis is guarded even with full mouth extractions.
- Repository steroids and antibiotics are not indicated in the treatment of stomatitis.
- The extraction of all teeth and subgingival root fragments is usually curative.
Month 4: Benign oral masses
Why is this important?
Peripheral odontogenic fibromas (POFs), gingival enlargements (Figure 4), and cysts are benign oral swellings. Peripheral odontogenic fibromas (formerly known as fibromatous and ossifying epulis) are benign, often slow-growing tumors arising from periodontal structures (gingiva, periodontal ligament, and bone). POFs can be further subclassified as peripheral odontogenic fibromas and acanthomatous ameloblastoma.
Figure 4: Multiple gingival enlargements in a boxer dog; the extensive left mandibular mass histopathology confirmed peripheral odontogenic fibroma.

Many oral masses enlarge over time, placing pressure and causing discomfort on the periodontal ligament space. Early intervention can be curative to alleviate the need for major oral surgery.
What to know
- Oral cytology examined before excision can create a surgical plan that alleviates the need for incisional biopsy.
- Excision with at least 1 cm clean margins renders an excellent prognosis.6
Month 5: Malignant oral masses
Why is this important?
Oral melanoma, fibrosarcoma, squamous cell carcinoma, osteogenic sarcoma, and plasma cell tumors are the most common malignant oral tumors in dogs. Squamous cell carcinoma is the most common oral tumor in cats.
Oral neoplasia accounts for 6-7% of all cancers in dogs, and 3% of all feline cancers.7 Because of the aggressive nature of malignant oral tumors, early intervention carries the best prognosis.
What to know
- Excision with at least 2 cm clean margins renders a guarded to good prognosis. (Figure 5)
- Rostral tumors carry a more favorable prognosis than caudal tumors.
- There is an oral melanoma vaccine administered by oncologists after debulking.
- Follow-up radiation therapy is often indicated after excision to clean up residual cancer cells.
Figure 5: Curative excision with greater than 2 cm clean surgical margins in all directions.
Month 6: TMJ disease
Why is this important?
Temporomandibular joint (TMJ) diseases in dogs and cats include ankylosis, luxation, osteoarthritis, congenital abnormalities, traumatic fractures, and neoplasia.
These often-painful conditions can severely hinder the ability of dogs and cats to eat, drink, groom, and vocalize, leading to chronic discomfort and a diminished quality of life. Early diagnosis and prompt treatment are crucial to avoid complications including jaw misalignment (Figure 6), bone erosion, and permanent nerve damage.
Figure 6: A 17-week-old kitten with traumatic malocclusion.

What to know
- TMJ ankylosis involves surgical intervention to free up the rostral mandible from the affected joint.
- Cranial dorsal TMJ luxation often can be cared for with a pencil or tuberculin syringe placed between the caudal cheek teeth accompanied by mouth closure to replace the luxated condyle in the glenoid fossa.
Month 7: Oral trauma
Why is this important?
Dental and jaw fractures are common because of fights, automobile accidents, and hard chew products owners buy for their dogs to relish. Unfortunately, dentoalveolar trauma often leads to damage, infection, and pain.
What to know
- Physical examination after mandibular trauma often reveals malocclusion resulting from the collapse of the rostral mandible toward the side of the injury in unilateral fractures. Dropped jaws (inability to close the mouth) occasionally occur from bilateral fractures.
- Fractures of the mandibular bodies can be classified as favorable or unfavorable. Favorable mandible fractures run dorsocaudal to ventrocranial. The upward pull of the masseter and temporalis muscles and the downward caudal influence of the digastricus muscle compress the fracture. Stabilization of the tension surface may be required for bony healing (Figure 7).
- Unfavorable mandibular fractures run from dorsocranial to ventrocranial, distracting the fracture fragments. The alveolar crest bone is considered the tension surface, while the ventral cortex is the compression surface. Fixation devices must be load-bearing since no natural mechanism for fracture reduction exists.
Figure 7: Noninvasive stabilization with suture and buttons.

Month 8: Oral pharyngeal inflammation
Why is this important?
Month 8 spotlights the interplay between oral health and inflammation (Figures 8A and 8B), including gingivitis, contact mucositis, and stomatitis.
As in humans, oral inflammation in animals is painful. Chronic inflammation fuels bacterial invasion and threatens systemic health.
Figure 8A: Right vestibule inflammation secondary to contact mucositis.
Figure 8B: Left vestibule inflammation secondary to contact mucositis. Full mouth extraction resulted in resolution.
What to know
- Gingivitis (no loss of tooth support) treatment includes dental scaling, polishing, and irrigation followed by daily home care.
- For contact mucositis initial care, strict plaque control, pentoxifylline 20 mg/kg orally twice a day, and niacinamide at 250 mg orally twice a day are also helpful. Alternatively, extraction of the contacting tooth is usually curative.
Month 9: Broken teeth
Why is this important?
Tooth fractures are classified as complicated (exposed pulp) and uncomplicated (enamel or enamel and dentin exposed). Some tooth fractures also extend subgingivally (crown-root fractures). Understanding what to do for patients affected with traumatized teeth can be challenging due to the variations of presentation.
Complicated crown fractures create direct access of bacteria and oral debris to the pulp. Initially, the tooth will be sensitive.
What to know
- When the pulp is not exposed, and the dog or cat is an adult, generally nothing needs to be done unless there is radiograph evidence of periapical pathology.
- In a young—less than 2-year-old—dog or cat, the pulp is large, relatively close to the fracture site, and sensitive to heat, cold, and pressure. Tooth restoration is indicated in these cases.
- When the pulp is exposed, and the dog or cat is an adult, vital pulp therapy can be performed if the trauma occurred within a 48-hour window.8
Month 10: Choosing the right chew for your patients
Why is this important?
Maintaining oral hygiene in pets requires a multipronged approach, including methodical home care. Dental chews have become increasingly popular as a convenient option for at-home oral care, promising to remove or at least decrease plaque and prevent tartar buildup. With many brands, textures, and claims on the market, we face a critical task: helping our clients navigate the dental chew maze to choose the most effective options.
The first step in making informed recommendations is understanding the types of dental chews and their mechanisms of action. Common categories include the following:
- Abrasive chews, which typically feature complex textures, including rawhide, are designed to scrape away plaque and debris through physical chewing action.
- Enzymatic chews contain enzymes like lysozyme, which help break down and loosen plaque for easier removal.
- Dental treats often resemble regular treats and are formulated with plaque-reducing ingredients.
What to know
- Veterinarians and staff can influence their clients’ choice of safe and effective dental chews.
- The VOHC has accepted 72 dog and 17 cat products that decrease the accumulation of plaque or tartar.
Dental chews should be considered complementary tools, not replacements for other home care practices. Brushing remains the gold standard for oral hygiene, and it’s crucial to emphasize its importance alongside daily wipes and responsible chew selection—with an emphasis on VOHC acceptance.
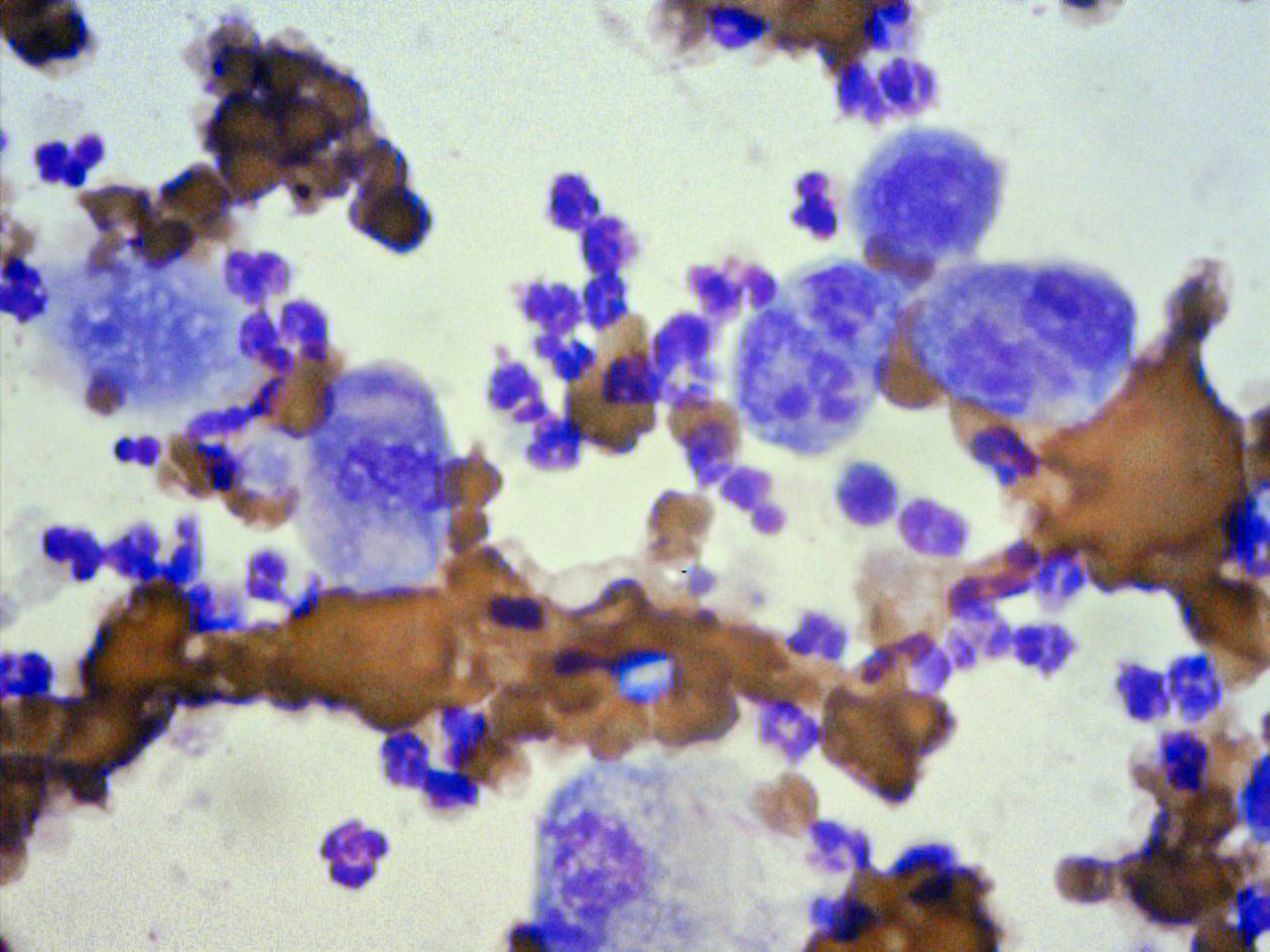
Month 11: Oral cytology
Why is this important?
Figure 9A: Cotton-tipped applicator used to obtain a cytologic sample.

Dogs and cats frequently present with swellings in the oral cavity. Cytology samples can be collected quickly, easily, and inexpensively (Figure 9A). Also, being less invasive than surgical biopsy, cytology gives rise to fewer complications. Based on cytology, lesions can be categorized as inflammatory (septic or nonseptic, granulomatous) or noninflammatory (hyperplastic, dysplastic, or neoplastic). If neoplastic, an attempt can be made to ascertain the origin of the cells present and to assess the degree of malignancy.
Collection techniques include fine needle aspiration and touch impression for ulcerated lesions.
What to know
- Positive results are considered positive; negative results may be a reflection of nonrepresentative sampling.
- Malignant criteria include at least 3 of the following: a population of cells in an abnormal location, variation in cell size and shape, increased cytoplasmic basophilia, large coalescing vacuoles within the cytoplasm, pleomorphic nuclei, increased nuclear/cytoplasm ratio, increased number of nucleoli, or pleomorphic nucleoli (Figure 9B).
Figure 9B: Cytologic criteria of malignancy include increased nuclear/cytoplasm ratio, nuclear and nucleolar pleomorphism consistent with squamous cell carcinoma.
Month 12: Elegant extractions
Why is this important?
Extractions can be challenging. By removing the crown, you have a bird’s-eye view to work each root circumferentially vs buccal exposure.
What to know
Elegant extractions step-by-step:
1. Local anesthesia is administered.
2. A No. 11 scalpel blade is inserted into the gingival sulcus and advanced apically 360° to incise the coronal periodontal ligament.
Figure 10: A surgical bur is used to create a moat around the roots of the mandibular first molar to ease the insertion of the wing-tipped elevator blade.
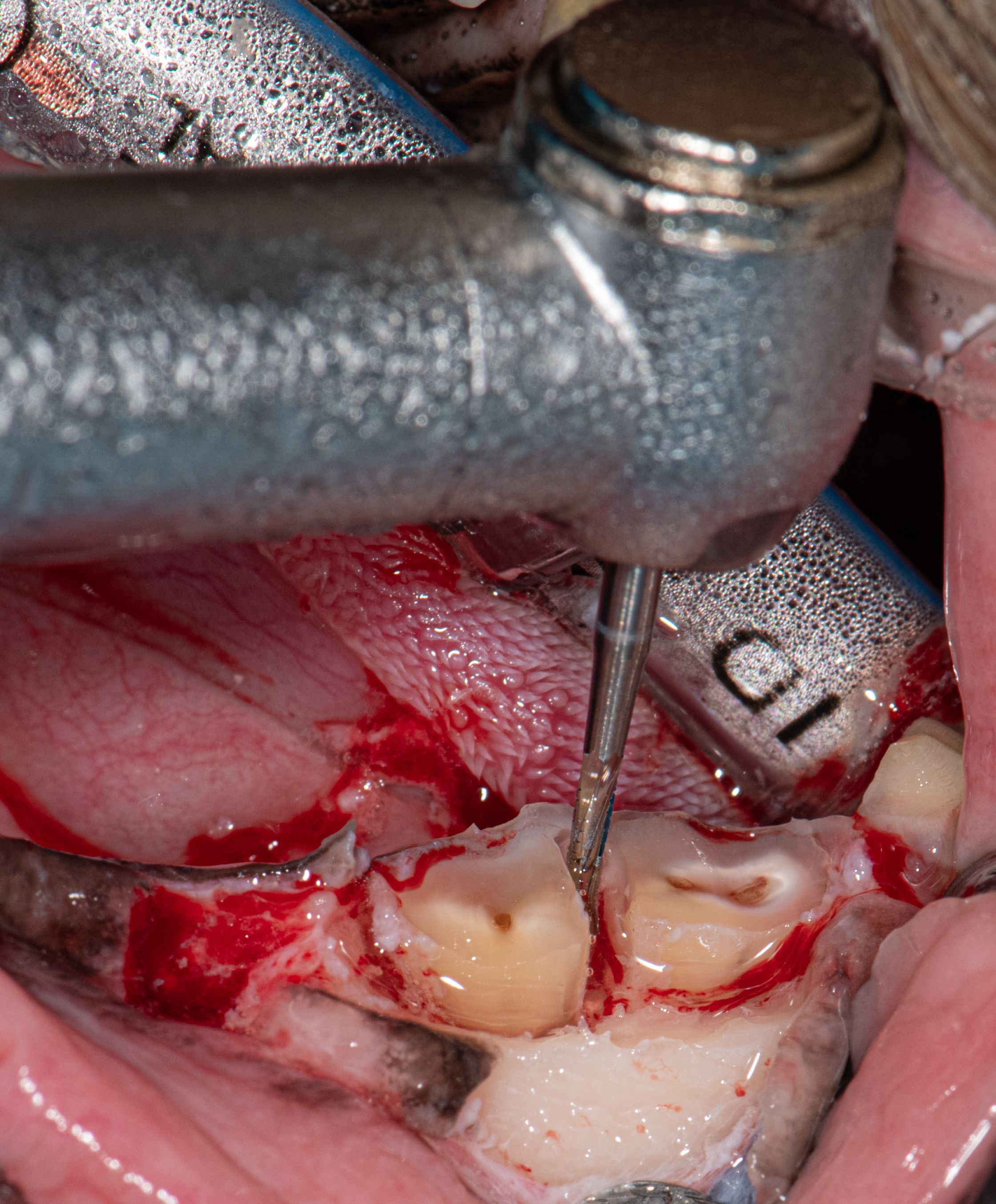
3. A buccal full thickness mucoperiosteal envelope or pedicle flap is created, including the surface mucosa, submucosa, and periosteum.
4. A No. 701 surgical tapered crosscut fissure bur is positioned horizontally at the cementoenamel junction to remove the crown. The crown is gently lifted off the roots using extraction forceps.
5. The No. 701 surgical tapered crosscut fissure bur is used to create a moat around the root(s) to facilitate the insertion of the sharpened wing-tipped elevator blade (Figure 10).
6. Moderate torsion is applied with an appropriate-sized wing-tipped elevator blade circumferentially until marked root mobility is created.
7. The football diamond bur clears the sharp alveolar crest before suturing.
8. The flap is enlarged, if needed, to facilitate tension-free closure.
Employing the philosophy of digesting the large dental meal 1 bite at a time, you will spend each month dissecting a discipline into understandable segments, facilitating a deeper understanding and more knowledge retention. Enjoy the journey!
Jan Bellows, DVM, DAVDC, DABVP, FAVD, received his undergraduate training at the University of Florida and his doctorate in veterinary medicine from Auburn University. After completing an internship at the Animal Medical Center in New York, New York, he returned to Florida, where he practices companion animal medicine surgery and dentistry at All Pets Dental in Weston. He has been certified by the American Board of Veterinary Practitioners (canine and feline) since 1986 and the American Veterinary Dental College (AVDC) since 1990. He was president of the AVDC from 2012 to 2014 and is president of the Foundation for Veterinary Dentistry from 2016 to 2024.
References
1. Enlund KB, Rahunen N, Thelander S, Olsén L. Evaluation of a thiol-detection test to assess tooth brushing efficacy in dogs. J Vet Dent. June 22, 2023. doi:10.1177/08987564231179898
2. Twice a year for life! American Veterinary Medical Association. September 1, 2004. Accessed February 4, 2024. https://www. avma.org/javma-news/2004-09-15/twice-year-life
3. Carrozza A. Tooth resorption in cats and dogs. dvm360. November 17, 2020. Accessed January 23, 2024. https://www. dvm360.com/view/classifying-tooth-resorption-in-cats-and-dogs
4. Lommer MJ, Verstraete FJ. Prevalence of odontoclastic resorp- tion lesions and periapical radiographic lucencies in cats: 265 cases (1995-1998). J Am Vet Med Assoc. 2000;217(12):1866-1869. doi:10.2460/javma.2000.217.1866
5. Hennet P. Chronic gingivastomatitis in cats: long-term follow-up of 30 cases treated by dental extractions. J Vet Dent. 1997; 14(1):15-21. doi:10.1177/089875649701400103
6. Berg J. Principles of oncologic orofacial surgery. Clin Tech Small Anim Pract. 1998;13(1):38-41. doi:10.1016/S1096-2867(98)80025-X
7. Cray M, Selmic LE, Ruple A. Demographics of dogs and cats with oral tumors presenting to teaching hospitals: 1996-2017. J Vet Sci. 2020;21(5):e70. doi:10.4142/jvs.2020.21.2e70.
8. Luotonen N, Kuntsi-Vaattovaara H, Sarkiala-Kessel E, Junnila JJ, Laitinen-Vapaavuori O, Verstraete FJ. Vital pulp therapy in dogs: 190 cases (2001-2011). J Am Vet Med Assoc. 2014;244(4):449-59. doi:10.2460/javma.244.4.449