Examining mandibular problems in a dog
Chronicling the progression of periodontal bone destruction resulting in mandibular fractures in a dog.
A neutered male rescued Shih Tzu of unknown age was brought to the referring veterinarian for a wellness evaluation. Oral examination showed generalized severe tartar, halitosis, gingivitis and gingival recession.

Dr. Brett Beckman
Full-mouth radiographs revealed generalized stage IV periodontal disease. Both mandibles were severely affected adjacent to the molar and premolar teeth. The referring veterinarian successfully performed multiple extractions (Photo 1). However, a bony swelling on the ventral aspect of the mandible adjacent to the mesial aspect of the right mandibular first molar (tooth 409) prompted referral to my facility.

Photo 1: A radiograph of the left mandible after extraction of the premolars and molars by the referring veterinarian. (PHOTOS COURTESY OF DR. BECKMAN)
An appointment was scheduled for later that month.
According to the clients, the patient did well three days after the extractions by the referring veterinarian. But on the third day, he escaped and roamed unattended outdoors for a few hours before he was found. For the next two days he was anorectic. The patient was brought back to the referring hospital, and a right mandibular fracture was found in the region of the previously noted swelling. Referral was then expedited to our next available appointment.
Patient evaluation and diagnosis
On examination of the patient at our practice, palpation was consistent with a right midbody mandibular fracture. Bony enlargement was present on the lingual and vestibular portion of the mandible surrounding the fracture site. The patient would not tolerate oral examination and was anesthetized for a dental radiographic examination, which confirmed a right mandibular fracture bisecting the alveolus of the mesial root of the first molar (Photo 2).

Photo 2: A radiograph of the right mandible demonstrating the fracture at the time of presentation to our practice.
Neoplasia is always a consideration, but the radiographs suggested a characteristic infrabony defect mesial to the mesial root of tooth 409 at the fracture site characteristic of a periodontal cause. Periodontal bone loss was severe in all four quadrants, further supporting a periodontal etiology. It is likely this patient had a pathologic mandibular fracture in the past with partial healing and stabilization. Concurrent focal osteomyelitis may also have played a role. In any case, this would create an ideal environment for refracture.
Treatment options
Edentulous pathologic mandibular fractures generally pose a challenge. In this case, tooth 409 required extraction before fracture repair, because leaving this tooth within the fracture line would beg failure. Traditional bone plates are usually poor options because of their intrusion on the mandibular canal and the presence of compromised bone density. External coaptation is generally futile for similar reasons. Interdental wiring or acrylic splints can be used to form the basis of primary repair only if adequate dentition is present surrounding the fracture site. Without teeth, creative measures are often needed to avoid mandibulectomy. In this case, a novel, malleable, titanium mesh material was chosen for primary repair.
Initial fracture repair
The mandibular first molar was extracted (Photo 3). An incision was created in the mucosa at the dorsal marginal bone to create a mucoperiosteal envelope flap. Thorough débridement and lavage restored normal bone and soft tissue margins. The inferior artery and nerve were not present within the mandibular canal, further confirming a preexisting fracture and partial stabilization.

Photo 3: A radiograph of the right mandible after extraction revealing the fracture.
The envelope flap was extended circumferentially around the ventral mandible to allow placement of the titanium mesh. The mesh was passed under the mandible with the aid of a curved hemostat, and microscrews secured it in place (Photo 4). Because of excellent accommodation of the plate to the tissue, relatively few screws were needed to provide good stability. The mesh cradled the mandible and opposed the bone, thus providing stability and aiding in retention of the subsequent bone graft (Photo 5).
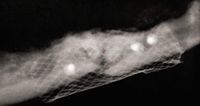
Photo 4: Titanium mesh surrounds the fracture. The bone graft consisting of autogenous bone and bone putty is visible within the defect.
Bone putty was mixed with cancellous bone harvested from the same mandible to create an osteogenic graft. The graft material was placed within the alveoli involved with the fracture, and the soft tissue was closed. An Elizabethan collar was placed on the dog while he was hospitalized. His appetite returned the same evening. On day three of hospitalization, the patient removed the Elizabethan collar—during the effort, he fractured the opposite mandible.

Photo 5: A radiograph of the left mandible after graft and titanium mesh placement.
Further repairs needed
Now faced with bilateral mandibular fractures in a patient edentulous caudal to the canines, what are our choices for repair?
Because of its novelty, an adequate amount of additional mesh material was not readily available. It also appeared this patient would be difficult to manage behaviorally to prevent further attempts to remove his collar or any repair device.
Part two of this three-part case study will detail a simple technique I and fellow veterinary dentists have used successfully as an aid in mandibular fracture stabilization. (P.S.: Were we successful in this case? A hint to the answer lies in the fact that this is a three-part series.)
Dr. Beckman is acting president of the American Veterinary Dental Society and owns and operates a companion-animal and referral dentistry and oral surgery practice in Punta Gorda, Fla. He sees referrals at Affiliated Veterinary Specialists in Orlando and at Georgia Veterinary Specialists in Atlanta, lectures internationally and operates the Veterinary Dental Education Center in Punta Gorda.