Early detection of chronic kidney disease (Proceedings)
Renal damage and disease can be caused by acute or chronic insults to the kidney.
Renal damage and disease can be caused by acute or chronic insults to the kidney. Chronic kidney disease (CKD) can be caused by diseases/disorders that affect any portion of the nephron, including the glomerulus, the tubule, the vascular supply, and surrounding interstitium. Early detection of CKD, prior to the onset of renal azotemia and chronic renal failure (CRF), should facilitate appropriate intervention that could stabilize renal function or at least slow its progressive decline.
Early Detection of CKD
Most acquired (vs. hereditary or familial) canine and feline CKD and CRF occurs in middle to older aged patients. An annual health examination, that includes a complete blood count, serum biochemistry profile, and urinalysis, is one of the best ways to detect declining renal function (Table). Special attention should be paid to decreases in appetite, body weight, packed cell volume, and urine specific gravity. Conversely, increases in serum urea nitrogen, creatinine, and phosphorus, or urinary excretion of protein or albumin may indicate the onset of renal disease. The value of these individually nonspecific parameters increases when they are considered as a group. Plotting the inverse of the serum creatinine concentration vs. time can demonstrate a decrease in renal excretory function; the steeper the slope, the more rapid the functional decline. Developing a data flow charts is a excellent way to keep track of changes in body weight and clinicopathologic values. Longitudinal assessment of serum creatinine for example can indicate declining renal function even when values remain in the normal range. A serum creatinine concentration of 1.2 mg/dl may be overlooked on a single biochemistry profile, however if previous results showed a serum creatinine concentration of 0.6 mg/dl, ≥ 50% loss of renal excretory function may have occurred. It's important to keep in mind that hydration status and muscle mass can influence serum creatinine concentrations; concurrent assessment of urine specific gravity and body condition will aid in the interpretation of serum creatinine concentrations. Dogs and cats may also become more susceptible to bacterial urinary tract infections as their kidney function declines. If any of the above parameters suggest the possibility of renal disease, an ultrasound examination may be indicated to evaluate kidney tissue architecture. Pyelonephritis, renoliths, and renal cortical fibrosis can be demonstrated by ultrasound. Percutaneous or ultrasound-guided renal biopsy can also be utilized to confirm or further define renal cortical disease in selected cases.
Importance of Proteinuria as a Marker of Early CKD
Persistent proteinuria with an inactive urine sediment has long been a recognized clinicopathologic hallmark of CKD in dogs and more recently in cats. Beyond this diagnostic marker utility, the potential for proteinuria to be associated with the progression of CKD has also been recognized in dogs and cats. The implication that proteinuria may be a mediator of renal disease progression has stimulated a discussion about what level of protein in the urine is normal. Development of species specific albumin ELISA technology that enables detection of low concentrations of canine and feline albuminuria has helped drive this reevaluation process.
Albuminuria and Microalbuminuria
Albuminuria accounts for the majority of urine protein in most CKD states. Microalbuminuria (MA) is defined as concentrations of albumin in the urine that are greater than normal but below the limit of detection using semi-quantitative urine protein screening methodology (conventional dipstick analyses). Urine albumin concentrations can be adjusted for various urine concentrations by diluting the urine to a standard specific gravity prior to assay (e.g., the Heska E.R.D.-Health Screen™ Urine test). Using urine that has been diluted to a specific gravity of 1.010, MA has been defined as a urine albumin concentration > 1.0 mg/dl but < 30 mg/dl. Albuminuria above this limit is referred to as overt albuminuria and can usually be detected using the urine protein/creatinine ratio (UP/C).
Causes of Microalbuminuria
Persistent MA reflects the presence of intraglomerular hypertension and/or generalized vascular damage and endothelial cell dysfunction in humans. Based on recent studies, MA appears to be a good indicator of early renal disease in dogs, particularly those diseases that involve the glomerulus. Albuminuria was evaluated in 36 male dogs with X-linked hereditary nephropathy, a rapidly progressive glomerular disease that is secondary to a defect in type IV collagen, a structural component of the glomerular basement membrane. In these dogs, ultrastructural lesions in the glomerular basement membrane become apparent by 8 weeks of age. In a longitudinal study, persistent MA was detected in dogs with X-linked hereditary nephropathy between 8 and 23 weeks of age, as much as 16 weeks before the onset of overt proteinuria. In another study of 12 healthy dogs that were experimentally infected with Dirofilaria immitis L3 larvae and evaluated over time, all of the dogs developed MA with 82% of all samples collected over the 14 to 23 month post-infection period of study being positive for MA. The onset of MA corresponded to the onset of antigenemia. The magnitude of MA increased over time and MA preceded the development of overt proteinuria, as measured by UP/C. At the end of the study, all of the dogs had histologic evidence of glomerular disease by either light or electron microscopy. Lastly, in 20 soft-coated wheaten terriers that were genetically at risk for the development of protein-losing enteropathy and nephropathy, the prevalence of MA was 76%. The magnitude of MA increased over time and 43% of the dogs with MA eventually developed abnormal UP/Cs. Significantly, persistent MA developed in these dogs at approximately the same time that mesangial hypercellularity and segmental glomerular sclerosis was observed histologically. The results of these three studies demonstrate the utility of MA as a marker of early CKD.
Similar to what is observed in people, MA is also observed in dogs and cats with systemic diseases that can alter glomerular permeability to plasma proteins. Inasmuch as the soft-coated wheaten terriers discussed above are predisposed to inflammatory bowel disease, the MA observed in some of the dogs that did not progress to overt proteinuria may have been caused by vascular inflammation secondary to the IBD, rather than progressive CKD. Other conditions have been reported in dogs with MA, including infectious, inflammatory, neoplastic, metabolic and cardiovascular disease. Results of a study of MA in dogs with lymphosarcoma and osteosarcoma demonstrated that urine albumin concentrations were significantly increased in dogs with these tumors, even though UP/Cs may not be increased above the reference range. Urine albumin concentrations did not, however, appear to consistently decrease with decreased tumor burden. The prevalence of MA in dogs admitted to ICU is higher than other reported patient populations and appears to vary with different classifications of disease. As reported in people with acute inflammatory conditions, transient MA occurred in some of these dogs. Conversely, a large percentage of dogs that were euthanized or died had MA suggesting, that as in people, the presence of MA may be a negative prognostic indicator.
Dogs and cats with persistent MA (i.e., MA present on 3 urinalyses > 2 weeks apart) are at greatest risk for CKD or systemic diseases that can adversely affect the kidneys. Similarly, MA that is not only persistent but increases over time should be of more concern than MA that is stable. The appropriate response to albuminuria/proteinuria should first be continued monitoring. In cases of persistent albuminuria/proteinuria and/or increasing albuminuria/proteinuria, further investigation is warranted and may include blood pressure measurement, imaging, serology, and biopsy. This investigation should be designed to rule out underlying/concurrent systemic diseases and to further define the CKD. Perhaps the best treatment for albuminuria/proteinuria is the identification and correction of underlying or concurrent disease processes. Dietary therapy (early renal failure diets) and angiotensin-converting enzyme inhibition have been recommended for treatment of persistent and/or increasing "idiopathic" albuminuria/proteinuria, however in the case of MA these treatments have not been evaluated in a prospective, controlled fashion.
Implications of Proteinuria and Albuminuria
In addition to the classic complications of persistent proteinuria (hypoalbuminemia, edema, ascites, hypercholesterolemia, hypertension, and hypercoagulability), there is increasing evidence in laboratory animals and human beings that proteinuria can cause glomerular and tubulointerstitial damage and result in progressive nephron loss. Proteinuria/MA can occur secondary to immune-mediated or structural glomerular damage or as a consequence of intraglomerular hypertension/hyperfiltration secondary to the compensatory hypertrophy that occurs in remaining viable nephrons in the face of any type of CKD. Plasma proteins that have crossed the glomerular capillary wall can accumulate within the glomerular tuft and stimulate mesangial cell proliferation and increased production of mesangial matrix. Proteinuria/MA can also occur secondary to tubular dysfunction that decreases the reabsorption of albumin and other proteins from the glomerular filtrate. By either mechanism, excessive amounts of protein in the glomerular filtrate can be toxic to tubular epithelial cells and can lead to interstitial inflammation, fibrosis, and cell death by several mechanisms. These mechanisms include tubular obstruction, lysosomal rupture, complement-mediated and peroxidative damage, as well as increased production of cytokines and growth factors.
Evidence linking proteinuria to progression of renal disease in dogs and cats is also beginning to accumulate. In dogs with the remnant kidney model of renal failure there is an association between proteinuria and individual nephron hyperfiltration. In 45 dogs with naturally-occurring CRF, the relative risk of uremic crisis and mortality was approximately 3 times higher in dogs with a UP/C ≥ 1.0 (n = 25) compared with dogs with a UP/C < 1.0 (n = 20). The risk of adverse outcomes was approximately 1.5 times greater for every 1 unit increase in UP/C. In addition, the decline in renal function, as measured by serum creatinine, was greater in dogs with higher UP/Cs. Similar findings have been observed in cats with the remnant kidney model of CRF where proteinuria was associated with nephron hypertrophy, intraglomerular hypertension, and glomerular hyperfiltration. In cats with naturally-occurring CRF, relatively mild proteinuria (UP/C > 0.43) was a negative predictor of survival. Interestingly, low level proteinuria, within the conventional normal reference range, also appears to be a predictor of survival in healthy, non-azotemic cats. In one study, the median UP/C for cats that died was 0.3, compared with a UP/C of 0.16 for cats that were alive at the end of the study or lost to follow-up. Finally, in dogs with naturally-occurring protein-losing nephropathies (x-linked hereditary nephritis in male Samoyeds and idiopathic immune complex glomerulonephritis) treated with angiotensin-converting enzyme inhibitors having renoprotective effects that decrease or delay progression of disease, a reduction in proteinuria was also observed.
In summary, proteinuria is a common disorder in the dog and cat that can indicate the presence of CKD prior to the onset of azotemia. Tests for MA can detect abnormal albuminuria at its earliest stage and appear to be valuable adjunctive tests for early detection of CKD. In addition to being a diagnostic marker of renal disease, proteinuria/MA may also contribute to the progressive nature of canine and feline renal disease.
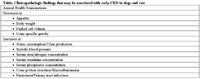
Table. Clinicopathologic findings that may be associated with early CKD in dogs and cats
Urinalysis offers a noninasive, rapid screening for canine cancer detection
February 9th 2024This is the first rapid test using urine developed by the Virginia Tech College of Engineering, College of Agriculture and Life Sciences, and the Virginia-Maryland College of Veterinary Medicine
Read More
Sweet pee new remedy in feline diabetes
November 9th 2023A novel class of drugs normalizes blood glucose in type 2 diabetic cats by dumping sugar into urine rather than modulating glucose uptake in the tissues but patient selection and close monitoring are crucial to using them safely
Read More