Cytauxzoonosis: a treatable disease (Proceedings)
Cytauxzoonosis is a tick-transmitted protozoan disease of cats caused by Cytauxzoon felis that was first reported in Missouri in 1976. Over the next thirty years the disease was only recognized in the southcentral and southeastern United States. Recently the geographic range of the organism has been recognized to extend east and north.
History
Cytauxzoonosis is a tick-transmitted protozoan disease of cats caused by Cytauxzoon felis that was first reported in Missouri in 1976. Over the next thirty years the disease was only recognized in the southcentral and southeastern United States. Recently the geographic range of the organism has been recognized to extend east and north. The states in which C. felis has been reported are shown below.

Classification and life-cycle
Based on its DNA sequence and life-cycle, C. felis is closely related to the Theileria spp. Unlike Babesia spp. which have only been found to infect red blood cells, Cytauxzoon and Theileria first enter a white blood cell after tick-transmission to the vertebrate host. Below is a cartoon depicting the proposed life-cycle of C. felis showing Bobcats (Lynx rufus) as the most likely reservoir hosts. Dermacentor variabilis and Amblyomma americanum have been demonstrated to transmit C. felis to domestic cats under laboratory conditions. The disease typically occurs between the months of April and September which correlates with the peak tick activity in most regions. Approximately 13-16 days after being bitten by an infected tick the cat develops non-specific signs of illness, typically characterized by anorexia, lethargy, pyrexia, icterus, and pallor. The initial infection of macrophages, or schizogenous phase, is responsible for nearly all the pathology associated with cytauxzoonosis. Bobcats do not appear to undergo a profound schizogenous phase of infection and therefore do not develop severe clinical disease. The erythrocytic phase of the organism alone does not induce severe disease.
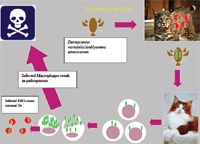
Proposed Life Cycle
Clinical signs and laboratory abnormalities
It is typically characterized by an acute febrile illness that is associated with decreases in one or more cell lines. Physical exam findings are often non-specific. Cats usually have a profound fever, but hypothermia may be identified in moribund cats. Lymphadenopathy and splenomegaly are common but not uniform findings. Cats are typically depressed and vocalization (death yowl) is a common finding in advanced cases. Some cats will have dyspnea as a prominent clinical feature (in our experience this is frequently due to pleural effusion and can be addressed easily with thoracocentesis). Laboratory abnormalities include non-regenerative anemia, leukopenia, thrombocytopenia, hyperbilirubinemia and bilirubinuria, elevations in liver enzymes (often not as severe as would be expected considering the degree of hyperbilirubinemia), hyperglycemia and hypoalbuminemia. In our experience thrombocytopenia and neutropenia are the most common CBC findings. Elevations in aPTT and non-overt DIC seem to be common. Many of the typical laboratory abnormalities become more pronounced as the disease progresses and may be absent or mild if the cat is presented for care early in the course of illness. The course of disease is short, and most cats succumb within 5 days of the onset of clinical signs.
Risk factors
Cytauxzoonosis is most frequently identified in young outdoor cats. They often have a history of tick attachment. There appear to be "hot spots" of infection, and often more than one cat in a household or neighborhood will become infected. In some households where cytauxzoonosis has been diagnosed, the prevalence in the domestic cats may be >30%.
Diagnostic testing
Microscopy: Organisms in red blood cells are most easily identified on 1000X. Schizont infected macrophages can be seen at low power and can look like platelet clumps on the feathered edge of a peripheral blood smear. Fine needle aspiration and cytology of liver, spleen and lymphnodes can facilitate a rapid diagnosis in suspect cases. In house quick stains are usually adequate
Polymerase Chain Reaction: PCR testing can be sensitive and specific.
Treatment
Aggressive supportive care is a mainstay of therapy for cytauxzoonosis. This includes IV fluid therapy and anti-coagulants (unfractionated heparin 100-300U/kg SQ TID or 300-900U/kg IV as a CRI). Corticosteroids do not appear to have a negative effect on outcome but also do not seem to provide a benefit.
Atovaquone and Azithromycin
An atovaquone (15 mg/kg PO TID with a fatty meal) and azithromycin (10mg/kg PO Q24) drug combination is the current treatment of choice for cytauxzoonosis. A feeding tube should be placed at admission to facilitate administration of medications. A randomized clinical trial demonstrated survival rates of 60% for atovaquone and azithromycin compared to 27% for imidocarb dipropionate. Treatment should be initiated within hours of admission and should be started empirically for suspect cases in endemic areas even if a definitive diagnosis is not made easily.
Imidocarb diproprionate
Imidocarb diproprionate (Imizol®, Schering-Plough) 2-4mg/kg IM once. Repeat dose in 2 weeks. Side-effects include pain at injection site and cholinergic effects (SLUD). Pre-treatment with atropine reduces cholinergic effects. Success rate have been reported to range from 0-50%.
Diminazene aceturate
Has been used with some success, but is not FDA approved or widely available in the US.
Follow-up:
Time to respond
The response to therapy is NOT immediate. Most cats begin to improve within 4-7 days.
Recovery
In our experience, cats that survive acute cytauxzoonosis have complete resolution of all clinical signs (following some cats for >4 years). However, they may have persistent infection with the red blood cell form of the parasites. It is unknown whether or not these cats can serve as a reservoir for infection. It is strongly recommended that all cats are kept indoors.
Follow-up testing
Serial blood counts are recommended until PCV, WBC, and platelet count return to within normal range. In our experience, all biochemical abnormalities have returned to normal within 2-3 weeks. Parasites may remain detectable by microscopy and PCR for years.