Can you rule out pancreatitis?
Yorkshire Terrier, 10-year-old, female spayed, 11.4 lbs.
Signalment:
Yorkshire Terrier, 10-year-old, female spayed, 11.4 lbs.
Table 1
Clinical history
The dog presents for anorexia, vomiting since yesterday, and drinking a lot. The dog lately has been eating supplemented lean ground beef. The dog has a history of diabetes mellitus, pancreatitis, seizures and an undersized liver.
Physical examination
The findings include rectal temperature 102.0° F, heart rate 130/min, respiratory rate 30/min, pink mucous membranes, normal capillary refill time, and normal heart and lung sounds. The dog shows 5 percent dehydration and depression. There is also a tender abdomen and the dog groans when palpated.
Laboratory results
A complete blood count, serum chemistry profile and urinalysis were performed (Table 1).
Radiographic review
Survey thoracic and abdominal radiographs are done. The thoracic and abdominal radiographs are normal.
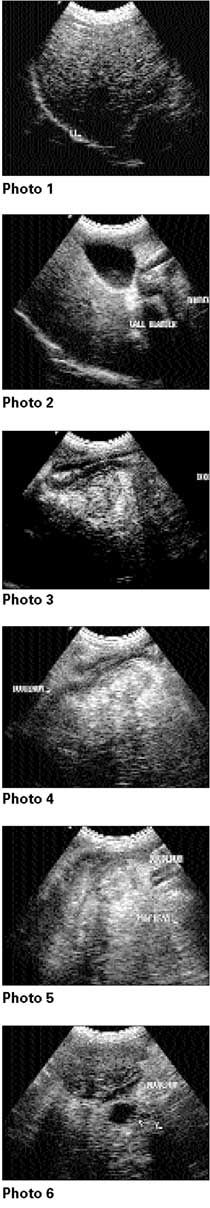
Ultrasound examination
Thorough abdominal ultrasonography is performed with the dog positioned in dorsal recumbency for the ultrasonography.
My comments
The liver shows uniform echogenicity. No masses noted within the liver parenchyma. The gallbladder is mildly distended, and its walls are not thickened or hyperechoic. The gallbladder does contain a small amount of sludge material. The spleen has uniform echogenicity - no masses noted. The left and right kidneys are similar in size, shape and echotexture. No masses or calculi were noted in either kidney. The urinary bladder is distended with urine and contains some urine sediment material - no masses or calculi noted. The stomach wall appears to be normal. The pancreas is enlarged and shows a mixed echogenicity. There is an increased amount of echogenicity around the pancreas - highly suggestive of active pancreatitis. There are also at least two anechoic structures, which are benign cysts or enlarged regional lymph nodes.
Case management
In this case, active pancreatitis and diabetes mellitus are the clinical diagnosis. At this point, I would recommend doing ultrasound-guided fine needle aspirations of the pancreas for cytologic examination. I do not see anything at this point that I can call a cancerous lesion in the hepatic, duodenal or pancreatic areas. I believe if the dog is treated supportively with fluids, antibiotics and regular insulin until the dog is eating well, the dog will recover.
It will normally take about two to three weeks for this episode of pancreatitis to resolve at best, so be patient and just manage the dog on a day-by-day basis. Possible complications may include gastric/duodenal ulcerations, pulmonary thromboembolism, renal failure and DIC.
Review of pancreatitis in older dogs
Pancreatitis is caused by the activation of pancreatic digestion enzymes within the pancreas itself, resulting in severe inflammation, necrosis and metabolic abnormalities. Acute pancreatitis may occur as a milder edematous form or severe hemorrhagic form.
Repeated episodes of pancreatitis often lead to chronic pancreatitis, with fibrosis and subsequently exocrine pancreatic insufficiency and/or diabetes mellitus.
Affected dogs usually present with sudden onset of vomiting, anorexia and depression. Physical examination may reveal cranial abdominal pain and fever. Chronic pancreatitis occurs in dogs that are predisposed to repeated episodes of pancreatitis, such as dogs receiving long-term immunosuppressive therapy or a high-fat diet or dogs with persistent hyperlipemia.
Exacerbations of chronic pancreatitis may resemble acute pancreatitis. Older dogs with chronic pancreatitis are often asymptomatic and clinical signs only develop as severe pancreatic fibrosis ensues, possibly contributing to entrapment of the biliary tract as the bile duct courses to its duodenal opening.
Diagnosing pancreatitis
Diagnosis of pancreatitis includes evaluation of laboratory values and diagnostic imaging of the cranial abdomen. The most common laboratory findings include neutrophilia, azotemia and increased serum ALP, ALT and AST activities.
The specific tests available for the diagnosis of pancreatitis in dogs are serum amylase and lipase activities and possibly serum canine pancreatic lipase immunoreactivity assay.
Serum canine pancreatic lipase immunoreactivity values greater than 82.8 µg/L (normal range, 1.9-82.8 µg/L) are consistent with pancreatic inflammatory disease. Abdominal radiography may show loss of cranial abdominal detail, lateral displacement of the duodenum, and abdominal and/or pleural effusion.
The pancreas is identified ultrasonographically with some difficulty in older dogs, requiring high-resolution equipment and careful attention to transducer position. In large, obese or deep-chested dogs, or those with signs of abdominal pain, it can be difficult to find an ultrasonographic window to the pancreas.
The left lobe may be visible between the stomach and transverse colon from a ventral or left lateral approach by the transducer. The right lobe is best visualized from a right lateral approach using the transducer to indent the abdominal wall to displace the small intestine and to bring the area of interest into the focal zone of the transducer.
Table 2
Once the duodenum is located, the right lobe of the pancreas may be visible dorsomedial to it. The right pancreatic lobe is normally hyperechoic when compared to the adjacent liver parenchyma. The pancreaticoduodenal vein passes through the right lobe and is visible in some instances, providing a useful landmark.
Ultrasonography of the cranial abdomen may then show a visualized enlarged pancreas with adjacent hyperechoic fat, pancreatic mass formation (secondary to peripancreatic fat necrosis), pancreatic pseudocysts and abscesses in the region of the pancreas.
Therapy for dogs with moderate to severe pancreatitis, intravenous fluid therapy at doses calculated to meet rehydration, maintenance, and ongoing losses should be provided. The fluid therapy should maintain normal blood pressure, replace losses induced by vomiting or exudation into body cavities and maintain a blood flow through the devitalized pancreas.
To assist in stabilizing systemic blood flow intravenous colloids may be administered such as hetastarch or dextrans at 10 to 20 ml/kg given more than one to two hours. Food should be withheld until the dog has not vomited for 24 hours; then water is provided in small amounts, followed by small amounts of a bland diet.
If no vomiting occurs, a bland diet (i.e. containing minimal fat and fiber, with moderate quantities of easily digestible carbohydrates and proteins) can be fed for several days before a gradual shift to an appropriate diet.
Other therapies used for pancreatitis include analgesic (butorphanol) and antimicrobial agents (ampicillin or a cephalosporin). Although pancreatitis itself is seldom a bacterial disease, the devitalized pancreas and peripancreatic fat, along with the localized peritonitis, can create a site for bacterial growth.
Ursodeoxycholic acid and antioxidants, such as vitamin E, may also be administered during clinical recovery from pancreatitis and in those dogs that have experienced recurrent episodes of pancreatitis.
Severe pancreatitis may also require the use of peritoneal lavage to reduce the caustic effect of pancreatic enzymes within the abdominal cavity.
Complications of severe pancreatitis can include pancreatic and peripancreatic mass formation (with the mass composed of necrotic pancreatic and omental tissue), pancreatic abscess formation and biliary obstruction.
Surgical intervention necessary for treatment of pancreatic masses or abscesses is often unsuccessful, and most dogs with these conditions die. Severe extrahepatic bile duct obstruction induced by fibrosing pancreatitis may also necessitate surgical intervention for a biliary diversion procedure.